Leukopenia
What is Leukopenia?
Leukopenia is a medical condition in which the number of white cells in the blood decreases, the risk for infection being increased. Also known as leukocytopenia, this medical condition presents several sub-types, depending on the type of white blood cells that are affected. One of the most encountered sub-types is neutropenia, a medical condition in which the number of neutrophils (a sub-type of white blood cells) are decreased. The neutrophil count is a good indicator for the risk of infection, as these are among the most numerous white blood cells.
In order to understand a medical problem such as leukopenia, you have to understand that the white blood cells in the blood are guardians of the immune system. These leukocytes are produced in the bone marrow by hematopoietic stem cells and their presences in the blood stream is considerably reduced (as time frame) than the one of the red blood cells. The different types of white blood cells are: neutrophils, eosinophils, basophils, lymphocytes and monocytes.
Leukopenia Symptoms
These are the most common symptoms of leukopenia:
- Fatigue
- Increased risk of bacterial, viral or fungal infection
- General weakness
- Fever and abdominal pain in more serious cases
- Pneumonia
- Appearance of blood disorders
- Sleepiness
- Increase of heart rhythm
- Shortness of breath, especially after effort
- Menorrhagia
- Headaches
- Irritability
- Hot flashes
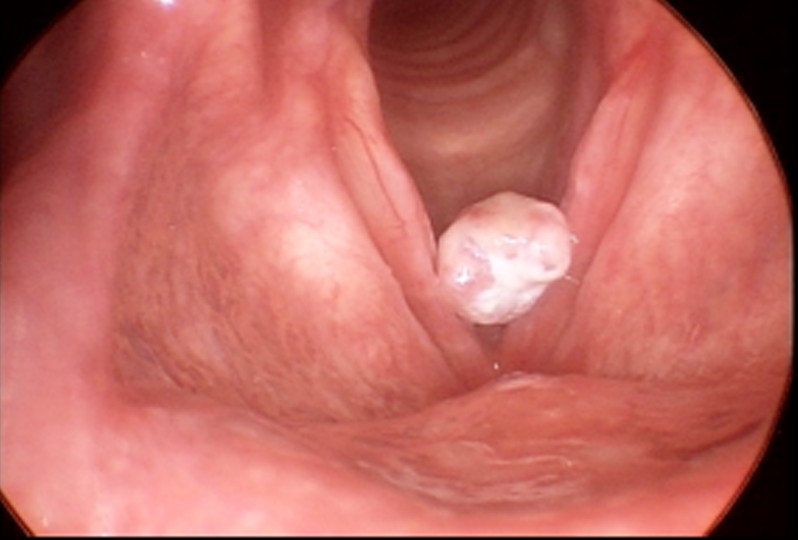
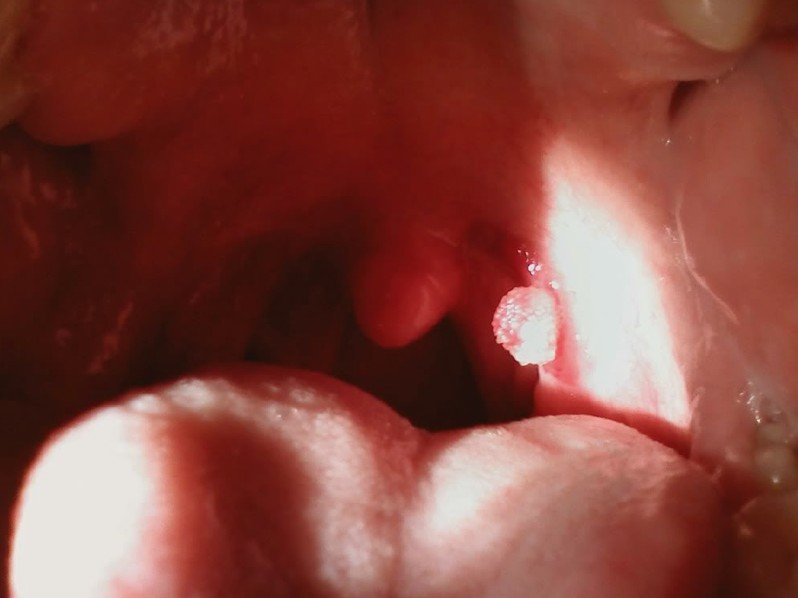
- Inflammation of the oral area – cheeks, lips, tongue, tonsils. This happens because the immune system is compromised.
- Inflammation of the stomach lining
- Ulcers
Leukopenia Causes
These are the most common causes of leukopenia:
- Medical conditions that interfere with the production or functioning of the bone marrow, as this is the place where white blood cells are produced
- Infections – viral, bacterial or fungal. It is a well known fact that infections of any sort will send the white blood cells into battle. Prolonged infections are equal to a decreased number of white blood cells in the bloodstream and a sure risk for secondary infections
- Autoimmune disorders – in this situation, the immune system attacks the body, producing antibodies. As the white blood cells are responsible for the immune system, you can certainly understand the connection between the two. For example, in the case of lupus, the body’s immune system attacks certain tissues and organs
- Congenital disorders – certain congenital disorders are accompanied by the lack of immunity. As the immune system does not function very well, there are few white blood cells fighting the possible infections
- Cancer – patients who suffer from different kinds of cancer need to undertake immune-suppressing therapies. This leaves them unprotected, as their white blood cell count is really low
- Chemotherapy and radiation therapy – these are often applied in cases of cancer and they contribute to the direct suppression of the immune system
- Prolonged treatments with antibiotics or diuretics – these can harm the immune system, causing a decrease of the white blood cells
- Anemia – this is a vicious circle, as low white blood cells cause anemia and anemia causes low white blood cells.
- Vitamin deficiency – if the body does not have enough vitamins, then the whole immune system is compromised and at risk for infection
- HIV/AIDS – this is a medical condition in which the immune system is at its lowest point, with really low numbers of white blood cells
- Thyroid disorders – hyperthyroidism. Hormonal imbalances, including the increased production of thyroid hormones can lead to the white blood cells to be reduced in number.
- Leukemia – as this is bone marrow cancer, the cancerous growth destroys the site where the white blood cells are produced and the immune system is 100% compromised.
- Infectious parasitic diseases – any parasite present on the body will be perceived by the body as an intruder and the immune system will work really hard to get rid of it, a lot of white blood cells being killed on the way.
- Rheumatoid arthritis – this is a systemic inflammatory disorder, with a clear influence over the immune system.
- Hypersplenism – this is a particular medical situation, in which the spleen is overactive and it basically kills the white blood cells.
Diagnosis
There are three basic methods for the diagnosis of leukopenia:
- Complete blood count – this is the easiest test in order to determine the number of white blood cells in the blood stream.
- Flow cytometry – this is an additional diagnosis test besides the blood count, recommended in cases leukemia is suspected.
- Bone marrow biopsy – this is a more advanced diagnosis test, used when the results of the complete blood count are inconclusive.
Treatment for Leukopenia
These are the most common courses of treatment for leukopenia:
- Corticosteroids – these are recommended in order to increase the white blood count in the blood stream
- Traditional medicine treatments are known to increase the production of white blood cells in the blood as well
- If the leukopenia is caused by certain medication that you are taking, such as diuretics, make sure that you reduce the dose or stop taking the medication altogether. Talk to your doctor about the alternatives you might have to this treatment, so that your white blood cell count is not affected
- If the leukopenia is caused by vitamin deficiency, then be sure to eat plenty of fresh fruits and vegetables. Also, you can take vitamin supplements, from the B complex and folate, copper and zinc
- In case of a bacterial infection, make sure that you take antibiotics for as long as the doctor prescribes them. If you stop taking them, then the bacteria will only become more powerful and it will develop resistance of the treatment, thus keeping your white blood cells to the lowest level possible
- Anti-fungal medication, administered orally and topically, is recommended for fungal infections
- Anti-viral medication in indicated in situations of viral infections
- Cytokine therapy can help to increase the white blood cell count