Superficial Spreading Melanoma
What is Superficial Spreading Melanoma?
According to the medical literature, this is one of the most encountered types of melanoma in the general population. Superficial spreading melanoma is a type of skin cancer, in which the pigment cells or melanocytes are transformed into malignant cells. It often affects more males than females and it is characterized by the fact that the malignant cells tend to stay within the initial tissue (epidermis). In many patients, the superficial spreading melanoma remains in the ‘in-situ’ phase for a long period of time, even decades.
In the initial phase, the superficial spreading melanoma grows on the surface of the skin in an horizontal manner. This is also known as the radial growth phase, when the skin presents lesions that are expanding (the area appears to be discolored). This type of skin cancer presents an increased risk to become invasive; the malignant skin cells can cross the border and breach into the other layers of the skin, including into the dermis (vertical growth phase). Such situations require aggressive treatments and the results are not always positive.
Symptoms
These are the most common symptoms of superficial spreading melanoma:
- The skin presents patches where there is discoloration. These patches extend with the passing of time but the growth is slow (several decades can pass before the patient notices the lesions).
- The patches of discolored skin are seen on the torso in males and on the inferior limbs in females.
- Often confused for other skin formations, such as freckles, moles or lentigo.
- They are already large in size when they are diagnosed, having a diameter of one or two millimeters.
- Their shape is irregular and the border is not always clear.
- They can have various colors (because of the different pigmentation), ranging from different shades of brown (lighter, darker) to black and blue, not to mention lighter shades of gray, pink or red.
- The discolored area might present streaks that have the color of the skin.
- When these lesions appear, their surface is initially smooth. As the time passes and the lesions become more distinctive, the surface becomes thicker, irregular and it is characterized by increased dryness.
- When the melanoma has breached the border and invaded other layers of the skin, the symptoms presented by the patient might be:
- Partial thickening of the discolored patch of skin
- More than one color present in the same area (often darker shades are noticed, including blue and black)
- There may be bleeding from ulcerating lesions
- The patient might feel a stinging sensation and also the need to scratch.
Causes of Superficial spreading melanoma
The main cause that leads to the appearance of superficial spreading melanoma is the development of pigment cells that are cancerous. These appear initially in the basal layer of the epidermis and they can breach this layer, entering the dermis. The interesting thing is that this type of cancer can appear on a healthy skin, without previous problems but in 25% of the cases it appears within an existing mole. This mole can be common but there are many situations in which the superficial spreading melanoma is linked to atypical, congenital or funny looking moles.
Specific gene mutations have also been incriminated as a direct cause and it seems that the damage caused by UV radiation (especially in case of sunburns and artificial tanning) is a cause of superficial spreading melanoma as well.
Besides the actual causes that lead to the appearance of this skin condition, there are certain risk factors that can add their contribution to the problem. These are:
- Age – as the superficial spreading melanoma develops over several decades, it seems that old age is a risk factor (however, the lesion has existed for some time and only then it was noticed and diagnosed).
- Existence of invasive melanoma or melanoma in-situ – patients who have already been diagnosed with such problems stand a high chance of receiving the same diagnosis all over again.
- Existence of other types of skin cancer
- Numerous moles of various colors and forms present on the skin. This becomes an even more obvious risk factor if there is constant and prolonged sun exposure
- Family history of melanoma
- Light skin and light colored eyes
Diagnosis
Superficial spreading melanoma can be diagnosed based on the clinical findings and the patient’s medical history. In the majority of cases, the dermatologist will first use a dermatoscope in order to take a better look at the lesion and then he will most likely recommend what is known as an excisional skin biopsy. The biopsy will be able to determine whether there are malignant cells or not. If a lesion is thick (over one millimeter thickness), then additional investigations will be recommended (complete blood count, biopsy of lymph nodes and CT or MRI).
Treatment
When it comes to superficial spreading melanoma, the first choice of treatment is surgical removal of the lesion. The surgeon will also take some safety margins, removing some healthy tissue surrounding the affected area, to be safe. However, as postoperative treatment the doctor might recommend radiotherapy, to make sure that the tumor is gone completely. In cases of metastatic melanomas, it is highly recommended that the lymph nodes are removed as well.
Survival rate
The prognosis for the superficial spreading melanoma is poor if the lymph nodes in the area are swollen or if there are metastases affecting the brain, the bone, the lungs or other parts of the skin. It is important to understand that the superficial spreading melanoma that stays within its border is not dangerous; it becomes serious when that border is breached and malignant cells enter other layers of the skin. The thickness of the melanoma upon surgical removal is also a good indicator for the survival rate. This is why it is highly important to go to regular follow-up controls and make sure that the lesion has not progressed or, in case of removal, that it did not appear again.
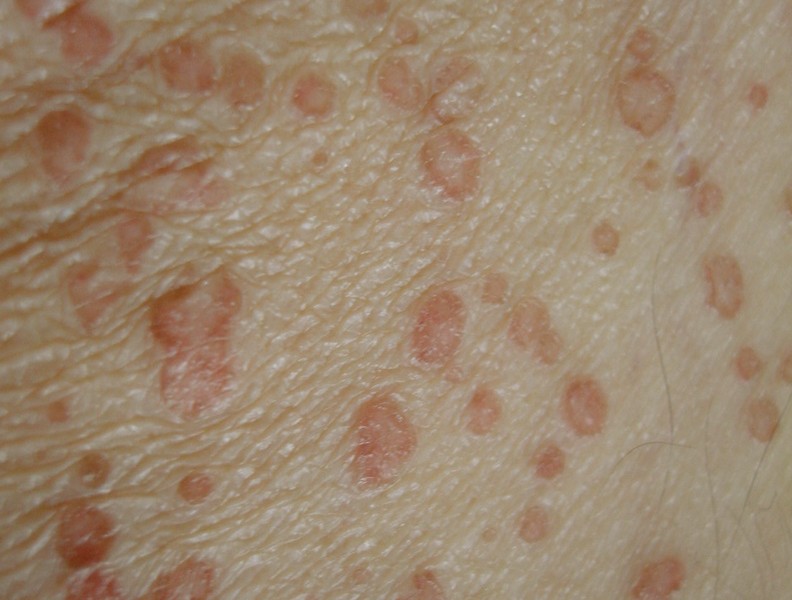
Pictures
Collection of photos, images and pictures of Superficial Spreading Melanoma…
















 This is recommended for whitening yellow nails, as the active substances contained in the lemon juice can act as bleaching agents. Squeeze some fresh lemon juice, put it into a bowl and soak your nails for a quarter of an hour. Then, use a soft brush in order to improve the color of the nails and scrub the yellow discoloration off. Rinse in warm water and apply a moisturizer made from natural ingredients. Repeat twice a day until the nails resume their natural color. The same process can be followed by using lemon essential oil, as an alternative to fresh lemon juice.
This is recommended for whitening yellow nails, as the active substances contained in the lemon juice can act as bleaching agents. Squeeze some fresh lemon juice, put it into a bowl and soak your nails for a quarter of an hour. Then, use a soft brush in order to improve the color of the nails and scrub the yellow discoloration off. Rinse in warm water and apply a moisturizer made from natural ingredients. Repeat twice a day until the nails resume their natural color. The same process can be followed by using lemon essential oil, as an alternative to fresh lemon juice. This is recommended because of its whitening properties but you need to be careful and use solutions that contain only 3% of this substance. The recommendation is that you mix the hydrogen peroxide with water and soak your nails for two minutes. Then, you will have to scrub them with a gentle toothbrush and rinse with warm water. You can also apply the substance directly to the nails, if the discoloration is severe and then follow the same process. Apply a moisturizer to prevent the skin from becoming dehydrated.
This is recommended because of its whitening properties but you need to be careful and use solutions that contain only 3% of this substance. The recommendation is that you mix the hydrogen peroxide with water and soak your nails for two minutes. Then, you will have to scrub them with a gentle toothbrush and rinse with warm water. You can also apply the substance directly to the nails, if the discoloration is severe and then follow the same process. Apply a moisturizer to prevent the skin from becoming dehydrated. This is recommended because of its whitening and exfoliating properties. One indication is that you mix baking soda with hydrogen peroxide and then apply the mixture on the yellow nails. You keep it for three or four minutes, then rinse in warm water and apply moisturizer. Another indication is that you mix baking soda with olive oil and fresh lemon juice, apply the mixture and leave it on for five minutes. The first procedure should be repeated every six to eight weeks, while the second every two weeks.
This is recommended because of its whitening and exfoliating properties. One indication is that you mix baking soda with hydrogen peroxide and then apply the mixture on the yellow nails. You keep it for three or four minutes, then rinse in warm water and apply moisturizer. Another indication is that you mix baking soda with olive oil and fresh lemon juice, apply the mixture and leave it on for five minutes. The first procedure should be repeated every six to eight weeks, while the second every two weeks. This is recommended especially when the yellow discoloration is caused by a fungus infection. Tea tree oil is a natural fungicide and it has amazing antiseptic and antimicrobial properties. You can use it to fight against the fungi infection and also to restore the natural color of your nails. Using an eyedropper, apply the tea tree oil for a few minutes, then rinse in warm water and apply moisturizer. This procedure should be repeated two times a day. Or, if you want, you can mix the tea tree oil with olive oil and apply it to your nails.
This is recommended especially when the yellow discoloration is caused by a fungus infection. Tea tree oil is a natural fungicide and it has amazing antiseptic and antimicrobial properties. You can use it to fight against the fungi infection and also to restore the natural color of your nails. Using an eyedropper, apply the tea tree oil for a few minutes, then rinse in warm water and apply moisturizer. This procedure should be repeated two times a day. Or, if you want, you can mix the tea tree oil with olive oil and apply it to your nails. This is recommended because of its antifungal properties. Mix the apple cider vinegar with warm water and soak your nails for about twenty minutes. Dry your nails with a soft towel and repeat the procedure at least three times every day.
This is recommended because of its antifungal properties. Mix the apple cider vinegar with warm water and soak your nails for about twenty minutes. Dry your nails with a soft towel and repeat the procedure at least three times every day.