Sweet Taste in Mouth
Have you been having sweet taste in mouth as if you took a sweet drink or licked some sugar? Do you experience a fruity taste that wouldn’t go away even after brushing? What you are experiencing is not new. A lot of people pass through similar experience without even understanding the cause of their problem.
There are several reasons why one experiences sweet taste in mouth. Whatever be the cause, the good news for you is that there are remedies for this condition. You can be treated and live your normal life again. In this post, we shall be sharing with you what sweet taste in mouth is, its causes, how to get rid of the condition, its relation with thyroid, etc. If you are currently passing through the experience or you have someone who is, then it is expedient that you pay attention to this post. Patiently read it to the end and make sure you share your concerns at the end, using the comment box.
Causes of Sweet taste in mouth
There are varied reasons why you experience sweet taste in mouth. We are going to look into few of the reasons why this phenomenon occurs.
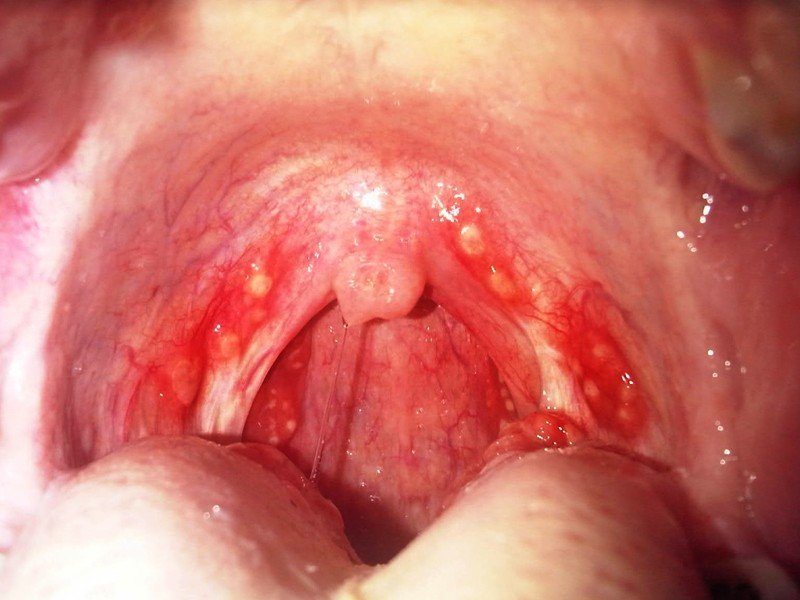
Pseudomonas infection
This results from infection caused by a bacterium known as pseudomonas. This infection leads to sinusitis (inflammation of the sinuses) and occasionally alters the taste buds thereby causing sweet taste in the mouth. A more severe infection would bring about impairment in the functions of the taste receptors. Further attacks by the bacterium could lead to swimmer’s ear and itchy nose. Pseudomonas can also infect the lungs where it produces cough with or without sputum production, fever, chills, and difficulty breathing.
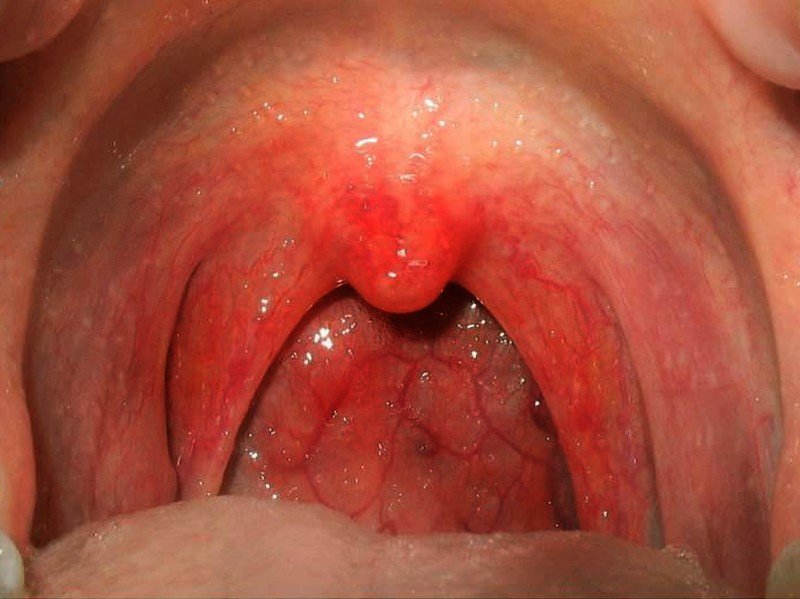
Indigestion
This symptom could come from acid reflux problem. When more acid is formed in the stomach, some acid are pushed back into the gut leading to sweet taste in mouth. Gastro Esophageal Reflux Disease (GERD) characterized by backup of particles of food into the mouth, with smell and taste of food. Other symptoms of GERD include chest pain and burning sensation in the stomach.
Diabetic neuropathy
Deposition of high blood sugar in diabetic disease as well as neuropathy that comes with condition can result in sweet taste in mouth. This can also be accompanied by dehydration and other symptoms. Sweet taste in mouth can persist even when the individual is fasting.
Epileptic attack
Some forms of epileptic attack, notably the grand mal, go through a warning stage (aura stage) which is characterized by unusual sound, flash of light, and taste in the mouth.
Diet
The type of diet you eat could be responsible for the sweet taste in your mouth. For instance if you ingest food containing artificial sweeteners like saccharin, there is the likelihood that you might experience sweet taste in the mouth hours after the main diet. Sometimes, you get the sweet taste after drinking water. So, before you start getting worried about what you are noticing, it is good to have a look at your diet again to be sure the taste is not coming from there. Foods with high sugar concentration can lurk around your mouth for a longer period. Sometimes, you can notice this taste after coughing especially if you have eaten the types of foods mentioned above.
Neurological disorder
The condition can also result from neurological disorder that may hinder the normal functioning of the nerve receptors that send out taste signals. The gustatory nerve (Glossopharyngeal nerve) is responsible for sending taste signals to the brain for interpretation. But when there is interference in the normal nerve signal resulting from nervous disorders such as seizure or stroke, this can affect the way you perceive taste. Serious degenerative nervous system disorders like Alzheimer’s disease, multiple sclerosis or Parkinson’s disease can also bring about a disturbance in electrical activities of the brain thereby impairing the normal functioning of the nerve responsible for sending gustatory signals. This can cause sweet taste in mouth.
Ketosis
When the body depends on fat for energy, the breakdown of the fats lead to the release of chemicals known as ketones. This condition is known as ketosis. Ketones also produce a byproduct referred to as acetone. It is this acetone that you breathe out, which is responsible for the fruity smell or taste that is experienced. Ketosis occurs in diabetes when there is a drop in the level of blood sugar and insulin. Conditions that give rise to drop in blood sugar level include going on weight loss diets with low carbohydrate and high protein contents, excessive exercise, anorexia (leading to starvation), etc. This is why there could be sweet taste in mouth after exercise or even when you are not exerting yourself physically.
Cancer
Some forms of cancer like lung carcinoma can lead to sodium depletion (hyponatraemia) due to the unbalance secretion of the antidiuretic hormone, a condition referred to as Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH). This distortion results in a situation in which all foods are interpreted as sweet. When the sodium distortion is corrected, the condition is reversed.
How to get rid of Sweet taste in mouth
Do you want to know how to get rid of sweet taste in mouth? Then you need to pay proper attention to everything we are going to discuss here. Below are some of the things you could do to reduce the unpleasant symptoms you are experiencing.
Get rid of acid reflux
Since GERD has been fingered as one of the causes of sweet taste in mouth, one way to treat the problem therefore, is to treat the GERD. This can be done by employing a combination of medications such as antacids (Aluminium hydroxide, Magnesium trisilicate), H2 receptor antagonists (ranitidine, nizatidine, cimetidine), Proton Pump Inhibitors (lansoprazole, omeprazole, esomeprazole), etc. They play a major role in helping to reduce acid reflux thereby reducing the symptoms of GERD.
Treat diabetes
Taking care of diabetes will also eliminate the sweet taste in mouth if it is associated with the disease. The type of drug to use for diabetes management depends on the type of diabetes, whether insulin-Dependent or Non-Insulin Dependent. For insulin dependent diabetes, the use of insulin helps to put the high blood sugar under control.
Non-Insulin Dependent diabetes would need multiple drug therapy like Metformin (Glucophage), and Glibenclamide (Clamide) or Chlorpropamide (Diabinese), etc for the control of blood sugar.
The above treatments can be augmented with exercises and change in diet. Some forms of regulated diets are prescribed for diabetic patients as medications alone are hardly sufficient to take care of the condition.
Treat cancer
The offending cancer can be treated with chemotherapy, radiation therapy or surgery depending on the stage of the cancer. When this is appropriately handled, the sodium imbalance can be restored or other measures can be specifically taken to correct the hyponatraemia which is responsible for the sweet taste in mouth. Temporary measures aimed at controlling the sodium imbalance would only produce temporary relief until the underlying cause is pragmatically addressed.
Antibiotics
Pseudomonas infection should be treated with the right antibiotics. It usually responds positively to one or more of the following antibiotics – Ciprofloxacin or levofloxacin, ceftazidime, gentamicin, ureidopenicillins, carbapenems, cefepime and ticarcillin. It is good to run the necessary tests in order to determine the best antibiotics to use for the treatment of the infection.
Watch your diet
If the taste is coming from your diet, change the diet or try and rinse your mouth thoroughly after eating. This will get rid of those artificial sweeteners sticking to your tongue and gums. Avoid foods that contain high concentrates of sugar. In addition, avoiding concentrated sugars would also help put your blood sugar under control if you are a diabetic.
Alternative treatments
Sweet taste in mouth does not respond to orthodox treatment alone. It sometimes responds positively to alternative medicine especially when used to supplement the orthodox ones. However, you must be aware that alternative medicine may not be trusted when there are serious problems like diabetes type 2 and nerve damage. So, if you have ruled out the existence of the aforementioned disease conditions, you can now make use of any of the following alternative medicines:
- Probiotic: Probiotic supplement are highly useful for improving digestion. They are bacteria that are highly beneficial for the preservation of healthy intestines that eventually assist in proper digestion. Probiotic can be found in foods like sauerkraut, yogurt, miso soup, kefir and kimchi.
- Supplements: Supplements containing digestive enzymes are also useful for the management of problems resulting from indigestion. They assist the GIT in breaking down food and making digestion easier. You can easily order for any of them from online stores.
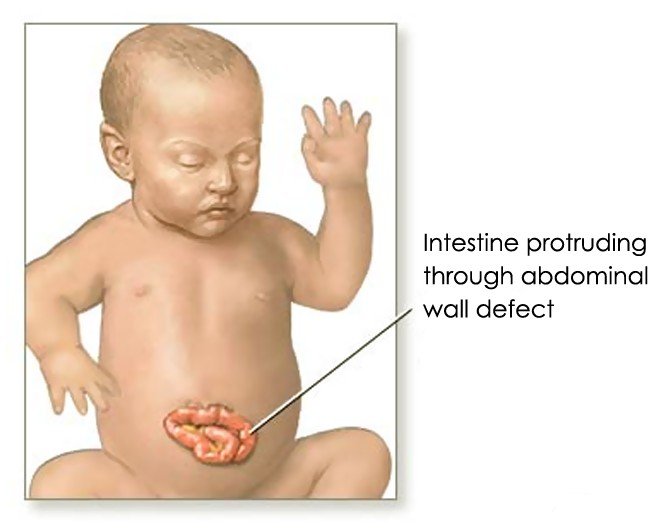
Sweet taste in mouth during Pregnancy
Occasionally, there could be sweet taste in mouth during pregnancy. Where this occurs, it is not an entirely strange phenomenon. A lot of women are known to experience metallic taste during pregnancy, which is oftentimes a sign of early pregnancy. This is one of the gustatory changes in early pregnancy.
However, some women have sweet taste in mouth during pregnancy as a result of gastrointestinal changes such as acid reflux. Like we noted earlier, when acid reflux occurs, some acid are pushed up into the gut leading to acid taste in mouth. This is the same way that the taste in mouth during pregnancy occurs.
This problem occurs in about seven percent of all pregnant women. The main prominent risk factors responsible for developing sweet taste in mouth during pregnancy include:
- A history of type 2 diabetes in the family
- History of previous pregnancy that resulted in gestational diabetes
- Obesity or overweight
- Being in pre-diabetic condition before pregnancy
- Previous history of pregnancy resulting in a baby with birth weight of 10 pounds (4.5kg) or more
- Being 25 years or older during the period of pregnancy
Though in majority of the cases the symptoms disappear on its own, it is advisable to see the physician to rule out pregnancy-induced diabetes mellitus which usually starts during pregnancy and is diagnosed during the same period.
Sweet taste in mouth in Early morning
Sweet taste in mouth in early morning can come from poorly controlled blood glucose in diabetics. Excess glucose gets deposited in between the gums/teeth thereby resulting in the sweet taste that you notice in the morning. This is one of the reasons while dental care is highly advocated for people suffering from diabetes.
The sweet taste in mouth in early morning often goes away after brushing. Sometimes, it gets less after drinking water, which helps to reduce the concentration of the sugar in the gums. In some cases, a visit to the dentist may be the first place to discover that you actually have diabetes even though the symptoms are not yet visible.
Relation with thyroid
Sugary taste in the mouth can be triggered by hyperthyroidism. In hyperthyroidism, there is an upsurge in metabolic rate which leads to carbohydrates being quickly used up by the body and an increase in the production of ketones and acetone. The acetone eventually results in sweet taste in mouth.
It is, therefore, not uncommon to see somebody with hyperthyroidism presenting with unusual sugary taste in the mouth. Other symptoms that may accompany this condition include hypersensitivity to heat, dehydration, nervousness, loss of concentration, weight loss, protruding eyes, rapid heartbeats, poor sleep, irritability, etc.
Conclusion
Sweet taste in mouth is a condition that results from different causes. When next you have such experience or you have a friend/relation who is going through it, remember to find out the exact cause before commencing any form of treatment. Where you are able to establish the cause of the problem, the treatments we have outlined in this post might be of help to you.
However, if for any reason your condition does not improve after trying the remedies, it is good to see the doctor for further investigations and proper medical management.