Achlorhydria
What is Achlorhydria?
Achlorhydria is simply the lack of hydrochloric acid in gastric secretions. It is seen as a secretion of acid, which at its maximum output, is less than 6.9m/mole/h on men and less than 5.0 m/mole/h in women.
Another definition sees achlorhydria as a condition whereby the serum pepsinogen I/pepsinogen II ratio is less than 2.9. Achlorhydria has been connected with intestinal metaplasia of the mucosa of the GIT, which may give rise to dysplasia. This is why it is regarded as a premalignant condition.
Symptoms of Achlorhydria
The cause notwithstanding, achlorhydria is known to be a product of bacterial overgrowth and intestinal metaplasia. Therefore, the symptoms are usually in tune with those diseases. Some of the noticeable signs and symptoms of this disease include:
- Gastroesophageal reflux disease
- Malabsorption of food
- Abdominal discomfort
- Bloating of the abdomen
- Stomach carcinoma
- Constipation
- Stomach infection
- Diarrhoea
- Anaemia
- Weight loss
Causes
This condition has diverse causes. Below are some of the popular causes of achlorhydria:
- A slow-down in Basal metabolic rate, as a result of hypothyroidism
- Excessive use of antacids or drugs that reduce the secretion of gastric acid (like H2 receptor antagonist), or drugs that slow down the transport of gastric acid (like proton pump inhibitors)
- Radiation therapy that involves the stomach
- Pernicious anaemia, where the body produces antibodies to attack the parietal cells that are in charge of gastric acid production
- It is a symptom of stomach cancer or atrophic gastritis
- It is also a symptom of Helicobacter pylori infection. Helicobacter usually causes a decrease in secretion and neutralization of the gastric acid in order to be able to survive in the stomach
- Gastric bypass procedures like duodenal switch which involves the removal or blinding of the largest acid producing parts of the stomach
- A deficiency of potassium, sodium, chloride, iodine and/or zinc, which are an essential part of stomach acid production
- It is a symptom of a rare disease like mucolipidosis (type IV)
- Sjogren’s syndrome: This is an autoimmune disorder which results in the destruction of many moisture-producing enzymes of the body
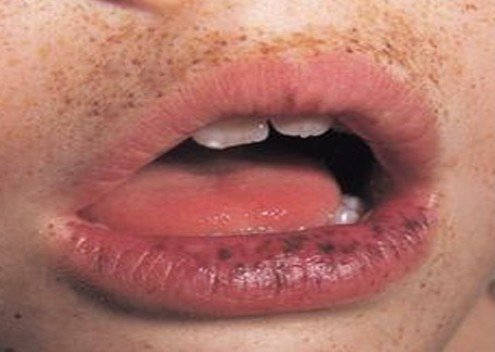
- It’s a sign of Pellagra, a condition which results from the deficiency of niacin
- Vipomas (Vasoactive intestinal peptides) and somatostatinomas which are both tumours of the islet cells of the pancreas.
Treatment
Achlorhydria can be treated in several ways. The inadequate secretion of gastric acid is usually as a result of some other underlying conditions. Therefore, in order to get a tangible result, those underlying causes need to be treated. We shall take a look at the different possible ways of taking care of this condition.
Treat Helicobacter pylori
This bacterium responds to a combination of antibiotics. The first line of antibiotics treatment include: proton pump Inhibitors (PPI) such as Omeprazole 20mg twice daily, plus Clarithromycin (500 mg twice daily), plus Amoxicillin (1g twice daily). In the case of patients who are intolerant to Amoxicillin, Levofloxacin (250 mg twice daily) can be used to replace Amoxicillin.
The duration of treatment is slightly different in the US and in Europe. European guidelines recommend a 7-day course of treatment, whereas the US recommends 14-day treatment. While there is a 12% higher success rate for a 14-day treatment, the rate of side effects also increases with prolonged treatment. It is also easier for patients to comply with a 7-day treatment.
Apart from the above triple therapy, the quadruple regimes can also be adopted. These include:
- Proton-pump inhibitor (PPI) + amoxicillin + clarithromycin + metronidazole
- PPI + amoxicillin or metronidazole + tetracycline + bismuth
- PPI + amoxicillin or tetracycline + furazolidone + bismuth
- The rate of resistance to furazolidone is relatively low. However, the drug is not readily available in all countries. It is currently unavailable in the UK.
Sequential therapy regimens:
- PPI + amoxicillin for 5 days, then PPI + metronidazole + clarithromycin or levofloxacin for 5 days (making a total of 10 days therapy)
- PPI + amoxicillin for 7 days, then PPI + clarithromycin + amoxicillin + metronidazole for 7 days (all making a total of 14 days therapy)
Treat bacterial overgrowth
Normal bacteria that reside in the wall of the gut do not cause any symptoms or problems. But bacterial overgrowth can result in bacteria colonizing over 100,000/ML in the upper gut. When this happens, the individual presents with symptoms like diarrhoea with malabsorption, D-lactic acidosis and a higher risk of endogenous infections.
An overgrowth of the bacteria of the small bowel also manifests with macrocytic anaemia, steatorrhoea, and enteropathy that result in protein loss. Microecologic changes also come with hypovitaminosis, B12 deficiency, protein deficiency, spread of bacteria and their toxins from the intestine into the bloodstream, etc.
To treat the bacterial overgrowth, therefore, you need to make use of antimicrobial agents like Amoxicillin/Clavulanate potassium, metronidazole, rifaximin, and ciprofloxacin. If you are not sure of the right dosage, see your doctor for advice. These drugs are prescribed in different doses for different conditions.
PPI dosage adjustment
Since Achlorhydria is known to result from long-term proton pump inhibitor (PPI) usage, it would be wise to reduce the dosage of the drug if the problem is traceable to it. Another wise thing to do is to completely withdraw the drug.
Gastric re-acidification
You can also correct Achlorhydria that is provoked by excessive use of PPI, by administering hydrochloric acid supplements like Betaine hydrochloride (BHCL). You can easily get it over the counter. Though BHCL has been proven to temporarily decrease the gastric pH in healthy volunteers with pharmacologically induced hypochlorhydria (Reduced secretion of gastric acid), stopping the PPI therapy is usually enough to stop the achlorhydria that is induced by medication.
Corticosteroid
Low doses of corticosteroid also help in reducing the inflammation of the parietal cells that are in charge of gastric acid production/secretion.
Pepsin
Pepsin has been used in medicine for a long time and is quite safe to use in assisting digestion. It is mostly used in combination with hydrochloric acid.
Surgery
This is the best way to treat carcinoid tumours. Surgical antrectomy helps in normalizing serum gastrin level and makes the multicentric gastric carcinoids to varnish as quickly as possible. Gastric resection can be used in treating patients with type I GI carcinoid tumours especially large-sized tumours. The success rate is quite high and encouraging.
Natural Remedies
Treatment of Achlorhydria also includes natural remedies. Some of the potent natural therapies are:
Herbs
Some supplements like grapefruit seed, oregano oil, enteric-coated peppermint oil and garlic are believed to play a vital role in helping to overcome bacterial overgrowth.
Ginger Tea
In traditional Chinese medicine and Ayurvedic medicine, ginger is regarded as tonic that aids digestion. Ginger helps in improving digestion and minimizing abdominal bloating.
Multivitamin
Achlorhydria is known to result in malabsorption of nutrients and consequently, in vitamin deficiencies. To correct these imbalances, multivitamins and mineral supplements are recommended. Adding the B12 vitamin is particularly advised in order to help compensate for the malabsorption of nutrients.
Bitter herbs
According to some alternative practitioners, bitter herbs may stimulate the stomach into secreting more acid and digestive enzymes. Some of the bitter herbs include gentian and dandelion, which are believed to aid the release of digestive juices. They are usually taken in capsule or liquid forms. You can also take herbal tea that has bitter herbs. You should drink a cup before food.
Peppermint
One major challenge with Achlorhydria is digestion problem due to the absence of gastric juice. But peppermint has the ability to aid digestion as a result of its antibacterial and gastric-acid-producing properties. It equally assists functions of digestion by reducing gas, improving bile flow, as well as healing the liver and the stomach.
Conclusion
Achlorhydria is caused by several factors and as such, it requires treating the individual root causes to be able to eliminate the problem. For Achlorhydria triggered by the use of certain drugs, stopping or reducing the dose of such drugs usually takes care of the problems.
However, we have listed drug therapies, natural remedies and surgery. If you are diagnosed with this problem, you will definitely find one of our recommendations useful. But whereby they fail to address your problem, it is advisable you see the doctor.