Brown Spots on Skin
When the skin is exposed for prolonged periods of time to the sun, the cells in the skin are multiplied. An increased in the number of melanocytes can lead to a darker skin but, in many cases, it causes the appearance of brown spots. These modifications on the skin are also known as age spots, as they often appear in the elder population. However, they are also presented as sun spots or liver spots, depending on the exact cause that has led to their appearance in the first place. Also, the treatment might be different according to the existence of an underlying medical condition.
The brown spots appear most often on the areas where the skin is directly exposed to the sun, such as the face, neck, chest and forearms. The back, the shoulders and, of course, the hands and the feet are often affected. The condition is more severe in patients who have had periods of prolonged exposure to the sun (for tanning or occupational purposes) and in those who have suffered from frequent sunburns. The elderly population is often diagnosed with brown spots on skin and it is seems that there is also a genetic predisposition to developing this condition.
The condition can be aggravated in cases of constant stress and anxiety, by pregnancy, in case of different types of vitamin deficiency and also in case the liver does not function properly. The good news is that these brown spots are harmless for the patient. Most of the patients seek out treatment and they try out different homes remedies because of the aesthetic concern.
What Causes Brown Spots on Skin?
These are the most common causes that can lead to the appearance of brown spots on the skin:
- Prolonged and constant exposure to ultraviolet
- Repeated artificial tanning
- The following are considered as risk factors:
- Light skin that rather burns than tans
- Frequent sunburns
Treatment
These are the most common treatments recommended for brown spots on the skin:
Topical applications
Bleaching cream – active substance: hydroquinone
Topical retinoids
These should be used only for reduced periods of time as a treatment, as they can have serious consequences on a person’s overall health
Corticosteroids
Topical corticosteroids of mild potency are recommended in this situation
Broad spectrum sunscreen
As the brown spots appear as a direct result of the prolonged sun damage, it is important to protect yourself from the sun and use sunscreen with high protection factor
Laser therapy/ intense pulsed light therapy
- Recommended to reduce the number of melanocytes in the skin
- The surface of the skin is not damaged
- Several therapy sessions are required before the first results are noticeable
- The skin might be slightly discolored after the therapy
- It is recommended that you use a high SPF sunscreen after undergoing laser or intense pulsed light therapy
Cryotherapy
- Liquid nitrogen is applied to the area with brown spots, freezing the melanocytes
- The results are noticeable after the skin heals
- Recommended to be used on single spots or on small clusters of brown spots
- Potential side-effects include:
- Temporary skin irritation
- Scarring (may be permanent)
- Discoloration
Dermabrasion
- This is a procedure in which the surface of the skin is practically sanded down with a specialized tool
- This will allow for a new layer of skin to form and it will take care of the brown spots
- Potential side-effects include:
- Treated area is red (temporarily)
- Scab formation
Chemical peel
- This is a procedure in which the surface of the skin is practically burned, with the help of a chemical substance
- After the chemical peel procedure, a new layer of the skin is going to appear and the brown spots will no longer be present
- Several sessions of chemical peeling are required before the results become noticeable
- It is recommended that you wear a high SPF sunscreen after you have undergone a chemical peel
- Potential risks include:
- Temporary skin irritation
- Discoloration
Home remedies
These are the most common home remedies you can try out for brown spots on the skin:
Lemon juice
- Direct application to the brown spots on the skin
- Applications of half an hour
- Cold water rinse after the application
- Daily repetitions until an improvement in skin appearance is noticed
- For sensitive skin, use water to dilute the fresh lemon juice
Buttermilk
- Application to the brown spots with the help of a cotton ball
- Applications of several minutes
- Cold water rinse after the application
- Can be combined with lemon juice for better results
- Daily repetitions are recommended until the first results are noticeable
Castor oil
- Recommended because of its healing properties
- Cotton ball applications
- Applications lasts several hours
- Cold water rinse after the application
- Daily applications (morning and night)
- Other types of oil you can use for the treatment of brown spots: vitamin E oil, coconut oil, olive oil, almond oil
Apple cider vinegar
- Mix with water, honey or orange juice
- Application lasts several minutes
- Cold water rinse after the application
- Daily applications are recommended
Aloe Vera
- Recommended because of its healing properties
- It can also be used to rejuvenate the skin after having undergone different therapies for brown spots
- Fresh Aloe Vera is indicated to be used through direct application
- Half an hour application
- Cold water rinse after the application
- Daily repetition of applications
Sandalwood
- Recommended because of its abilities to reduce excessive pigmentation
- It can be either used as a powder or as oil
Horseradish
- Direct applications to the skin as paste
- Alternative: mix with cider vinegar
Papaya
- Direct applications of fresh grated papaya
- Rinse and repeat daily
Yogurt
- Direct applications on the brown spots
- Cold water rinse
Onion juice
- Direct application of onion slices on the brown spots
- Daily repetition
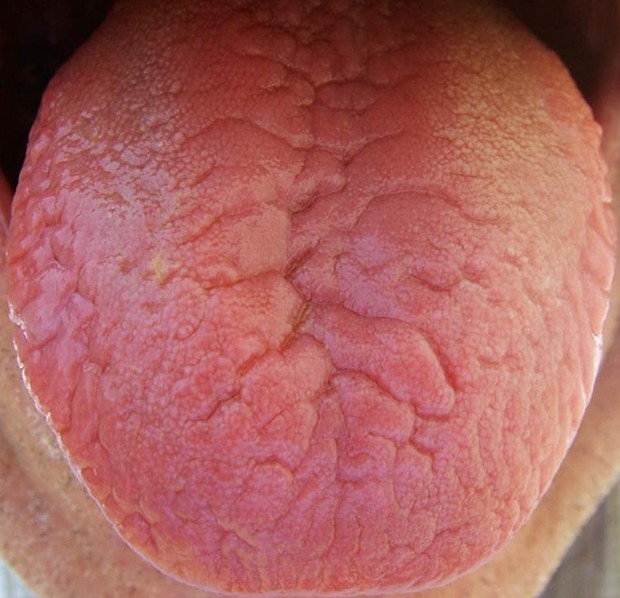
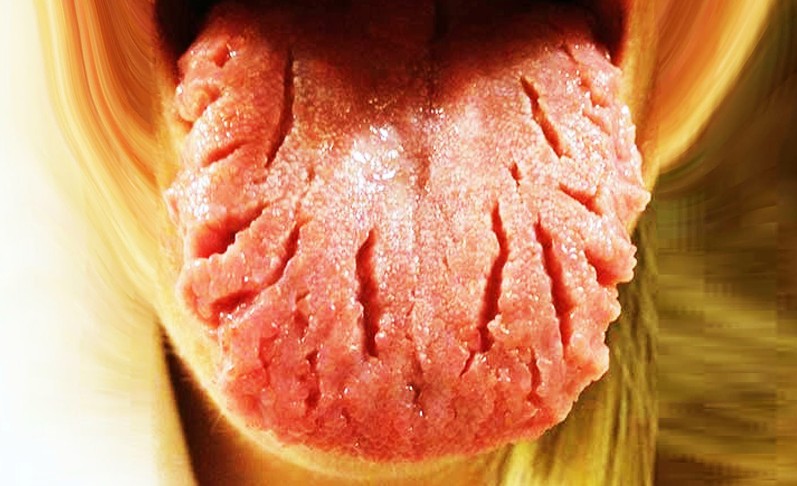
Pictures of Brown Spots on Skin
Collection of photos, pictures of brown spots on skin…