Cold Urticaria
What is Cold Urticaria?
Cold urticaria is a skin reaction to the cold temperatures, in which red and itchy bumps appear on the skin. The intensity of the symptoms depends on the actual stimulus (cold weather, cold object etc.) but also from one patient to the other, ranging from minor to severe reactions. This condition is most often encountered in young people, aged between 18 and 25 but it can also appear in children (as young as five years of age).
If cold urticaria develops for a period of more than six weeks, then it is diagnosed as a chronic condition. This allergy to the cold can persist throughout the entire life but it has no predictable course. It can be inherited (familial cold auto-inflammatory syndrome) or acquired. Also, there are different types of cold urticaria to be presented: primary (this appears when the patients come in contact with rain or cold objects, ice cubes included), secondary (this is rare, the patient presents serum abnormalities and association with purpura or Raynaud’s phenomenon), reflex (this is caused by the entire cooling of the body) and familial (this is the inherited one and the symptoms appear after exposure to temperatures below 22 degrees Celsius).
How common is Cold urticaria?
Cold urticaria is one of the most common conditions in which hives appear on the skin. However, it is said that this is a rare condition, affecting one in 1,00,000 people.
Symptoms
These are the most common symptoms of cold urticaria:
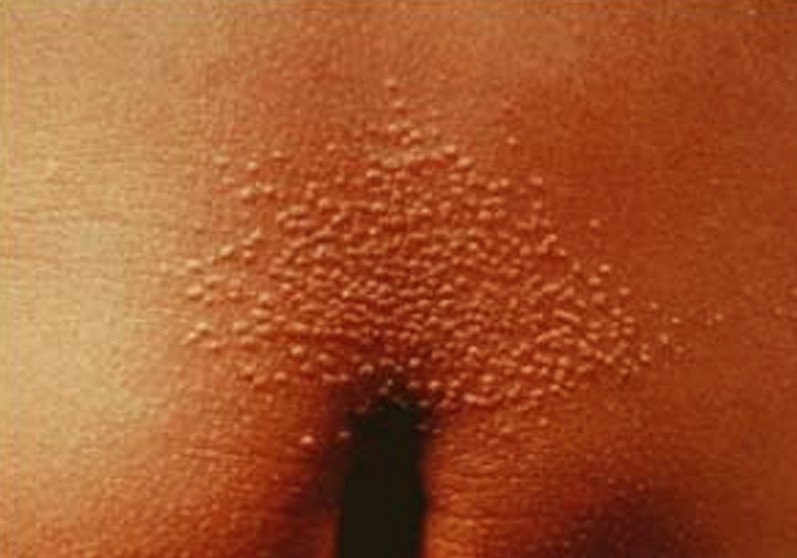
- Red and itchy bumps (hives) on the skin
- The hives are temporary and they appear on the areas that were exposed to the cold
- If the person goes from cold to warm, the skin reaction will aggravate
- Hands become swollen if a person holds a cold object
- Lips and throat become swollen if a person drinks cold beverages or eats cold foods
- In severe cases, the patient can present anaphylactic shock, with the following symptoms: syncope, rapid pulse, vascular collapse, airways closing in, tongue and lips swelling (difficult or impossible breathing). This requires immediate medical attention.
- Symptoms appear after immediate exposure to cold
- The skin is sensitive to temperatures below 4 degrees Celsius
- In some cases, the skin reaction is present to warmer temperatures
- Wind, rain and excessive humidity increase the risks for this condition
- Generalized skin reaction can appear after full body immersion in cold water
- Patients also describe a burning sensation along with the lesions on the skin
Causes of Cold Urticaria
These are the most common causes that lead to the appearance of cold urticaria:
- Sensitive skin cells (inherited condition, viral infection or other associated illnesses)
- Allergic reaction – the cold temperatures lead to the release of histamine from the mast cells
- Risk factors – age (children, young adults), infection (pneumonia), underlying pathologies (hepatitis, cancer), genetic (inherited condition)
- Idiopathic (unknown cause)
- General exposure to cold temperatures or cold water
- Hematologic conditions
- Underlying pathologies that have been associated with cold urticaria: cryoglobulinemia, chronic lymphocytic leukemia, lymphosarcoma, varicella, viral hepatitis, infectious mononucleosis.
Treatment
Cold urticaria cannot be cured but there is symptomatic treatment that you can follow. These are the most recommended treatments and indications for cold urticaria:
- Anti-histamines – these block the histamine release from the mast cells and they help with the itchiness and inflammation:
- Fexofenadine
- Desloratadine
- Ebastine (H1 anti-histaminic)
- Topical anti-histamine creams are also recommended but they are not as effective as oral treatments
- Other successful treatments:
- Leukotriene antagonists – these act against leukotrienes, which are compounds of the immune system (commonly recommended in allergies)
- Ciclosporin – this is an immunosuppressant recommended commonly for organ transplants but it has shown promising results in patients with cold urticaria as well.
- Systemic corticosteroids – these are recommended only for severe cases of cold urticaria and the treatment should be administered only for short periods of time, as it can have serious side-effects. Also, the treatment should be withdrawn gradually, as the patients can experience serious withdrawal symptoms when the treatment is stopped all of a sudden.
- Dapsone – this is an antibacterial drug that can help in cases of secondary infections.
- Oral antibiotics – these have helped patients with cold urticaria and bacterial infections.
- Danazol – this is actually a synthetic hormone.
- Doxepin – this is a drug commonly recommended for the treatment of depression and anxiety but it has shown promising results in treating the symptoms of cold urticaria.
- Omalizumab – this is a drug commonly recommended for the treatment of asthma but it has helped with the treatment of cold urticaria symptoms in patients who have not responded to other types of treatment.
- Patients are recommended to take with them an epinephrine auto-injector that can be used in case of severe anaphylactic reactions. Or, you can carry one of those medic alert bracelets.
- Avoid sudden temperature changes. Do not stay a lot of time in the cold and then enter all of a sudden into a warm room. Undress gradually and avoid putting your hands on a warm radiator or near a fire. This will only make the condition worse and it will accentuate the hives.
- Protect your skin from the cold. When going outside in cold temperature, be sure to protect the extremities by wearing gloves, scarf around the neck, warm socks and something on your head.
- If you are going to swim in cold water, then it is for the best that you wear an insulating wetsuit.
- Avoid drinking cold beverages and eating cold foods to protect your lips and throat.
- Avoid rooms with air conditioning (low temperatures).
- Desensitization of the skin – gradual and slow exposure to the cold, it can increase tolerance (for example, by taking regulate cold showers).
- Watch out for the factors that can aggravate the allergy to the cold, such as: excessive dryness of the skin, fabrics of the clothes that you wear (wool is a common culprit), laundry detergent or fabric softener used for the washing of the clothes and skin care products (most often, the soap you use leads to dry skin). By eliminating these aggravating factors, you can reduce the intensity of the cold urticaria.
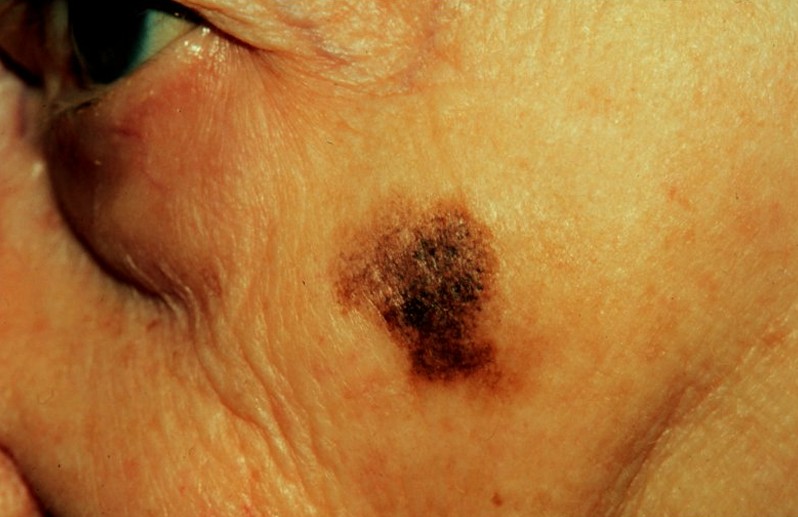
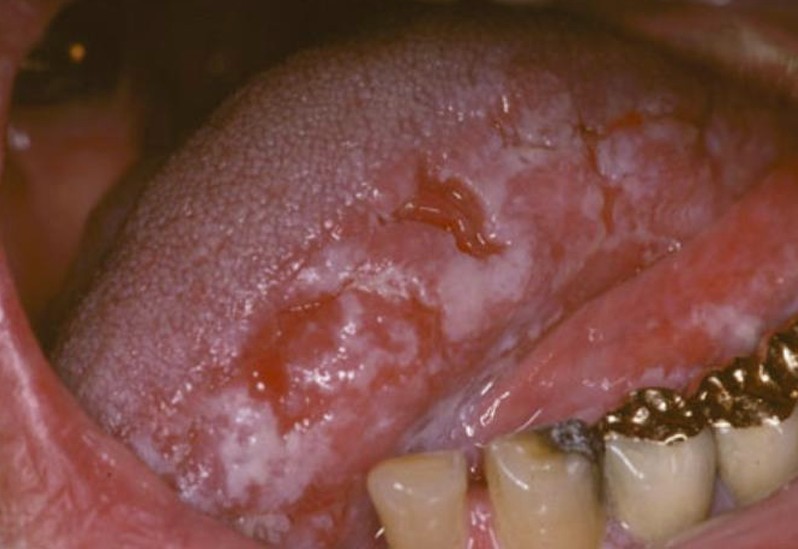
Cold Urticaria Pictures
Collection of images, photos and pictures of the skin condition Cold Urticaria…














 Levoscoliosis can appear under the following circumstances:
Levoscoliosis can appear under the following circumstances: