Prurigo Nodularis
What is Prurigo Nodularis?
Prurigo nodularis is an inflammatory skin condition characterized by the onset of itchy papules in the extremities. The itch and scratch cycle in prurigo nodularis results in the development of more papules.
Prurigo nodularis is often exhibited as multiple eruptions of excoriated papules on the surfaces of the limbs resulting from the incessant scratching. The more scratching made the more lumps will develop.
Prurigo nodularis is also known by another name such as Hyde prurigo nodularis and Picker’s nodules. The disease was first described in 1909 by Hyde and Montgomery describing the disease as itchy nodules on the extensor surface of the lower extremities. The disease was first described among middle aged women.
Prurigo nodularis is the most severe form of prurigo. This skin condition on the other hand is rather benign. Prurigo nodularis can affect the quality of life as the extent of pruritus and nodules can be debilitating and bothersome. The disease does not increase the chances of mortality except in the presence of underlying condition where the onset of prurigo nodularis is a secondary disease. There are cases where prurigo nodularis is being linked with a malignancy such as Hodgkin disease where prurigo nodularis is the manifestation of the primary disease. In modern day medicine, prurigo nodularis is regarded as the most common dermatosis in HIV patients where the incidence is deemed as a sign of severe immunosuppression.
The incidence of prurigo nodularis is found to be common among middle aged individuals and older adults although it can arise in any age group. No racial predilection has been recognized and the disease is deemed to occur in people worldwide. The frequency of the disease between sexes has not been fully recognized although there have been reports where prurigo nodularis is found to be prevalent among women.
Prurigo Nodularis Symptoms
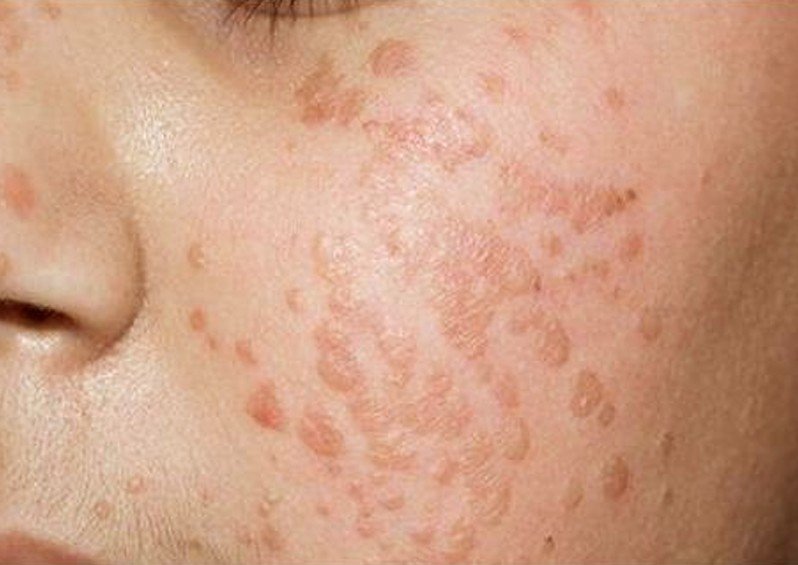
Prurigo nodularis is common among middle aged individuals and older adults although children may also get affected. It initially develops as a small and an itchy red bump on the extensor surface of the limbs. Prurigo nodularis causes an intense itching that provokes a vigorous scratching to relieve the itchiness. Scratching of the nodules however only intensifies the symptom of itchiness and only brings in more nodules.
The individual size of the nodule is about 1 cm to 3 cm in diameter and initially develops in the arms or legs although the nodules may develop in any part of the body. The nodules are discrete and appearing in hundred or two hundreds approximately and often appear in clusters and are symmetrically distributed. Excoriation of nodules is evident with a top that is flat and umbilicated or may have a crusted top. The crusty or scaly presentation of the nodules is due to the incessant scratching that brought the nodules to break off and sore. The color of the nodules may be purplish, reddish or brownish and the surface of the nodules is rough. The face and the palms can also get affected with nodules. The neck, upper arms and the shoulders can also be seen with nodules of prurigo nodularis with the cape of the neck as the most obvious area.
Itchiness is one of the hallmarks of prurigo nodularis along with the development of the nodules. The frequency of itchiness is so intense that it can distract the daily activities and can even disturb the sleep particularly at night time. The itchiness can also provoke a non-stop scratching to alleviate the itchiness although scratching can only make the condition worse. It only adds growth of new nodules while scratching can also cause the nodules to break off leading to sore that will cause the nodules to bleed. When the skin surface breaks off, it is highly potential for infection.
Long standing pruritus is the common complaint of patients with prurigo nodularis. The intensity of the pruritus causes the affected individual seems anxious, restless and worried. The disease usually lingers for a long time that it may cause depression and stress to the patient. Scratching does not provide relief, but only result in formation of new nodules whereas the old nodules do no resolve spontaneously. The old nodules will only leave a scar which can be darkly or lightly pigmented.
Prurigo Nodularis Causes
The exact etiology of prurigo nodularis remains unidentified. The pathophysiology of whether the lump or the itchiness occurred first remains vague as well. The exact cause of the inflammation and the formation of lumps and the amplification in the size of the nerve of the skin all remain unclear.
While the exact cause of prurigo nodularis remains unclear, several factors or conditions are considered to predispose the incidence of prurigo nodularis.
Atopic dermatitis
It is among the considered trigger of prurigo nodularis. Several numbers of patients reported to have a family history of atopic dermatitis prior to the development of prurigo nodularis.
Insect bites
Insect bite is considered a trigger of prurigo nodularis. The reaction to insect bites is believed to have perpetuated the itchiness and nodule formation.
Other conditions been linked to the onset of prurigo nodularis include the following:
- Immunodeficiency disorders including HIV
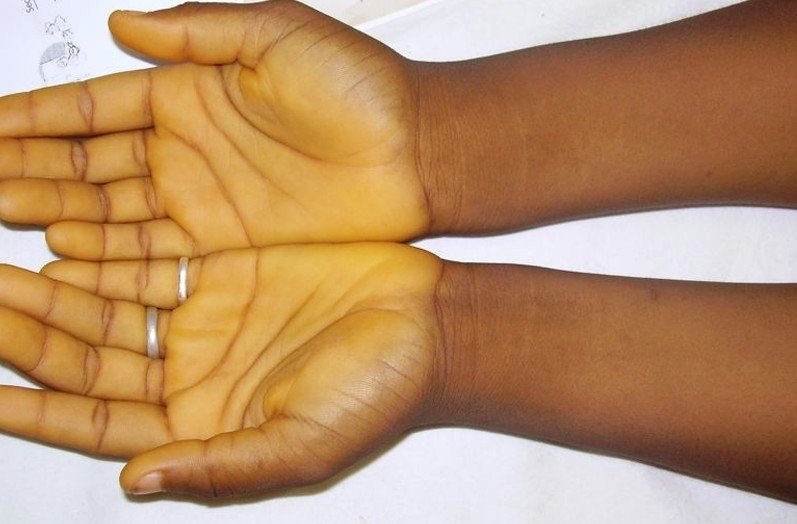
- Iron deficiency anemia
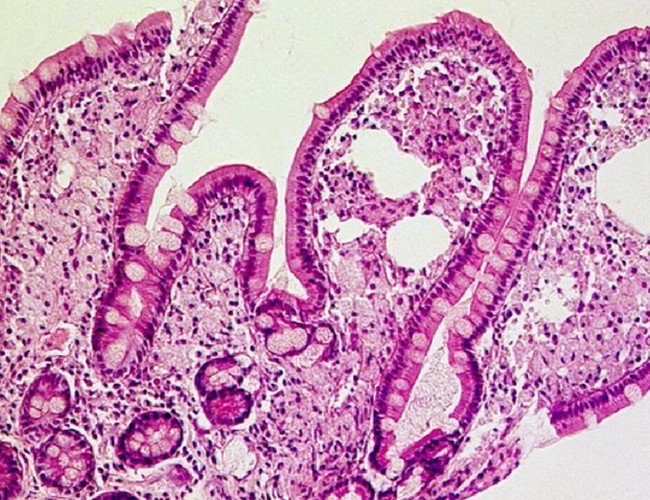
- Gluten enteropathy
- Malignancies
- Psychiatric illnesses
- Liver and renal dysfunction
Prurigo Nodularis Treatment
Prurigo nodularis is an inflammatory skin condition that is rather difficult to treat. It is considered as a resistant skin condition that the success of treatment is either mild or moderate. The challenge of controlling the disease is often done with a combination of medications.
The primary aim of treatment is to stop the patient from scratching which proves to be difficult on the part of the patient. Scratching only worsen the condition that it is necessary to alleviate the pruritus through medical means and not from scratching.
Treatments used to alleviate the itchiness and to reduce the inflammation and the lesions include the following:
- Antihistamines
- Corticosteroid
- Capsaicin cream
- Topical anesthetics
For more severe prurigo nodularis and for systemic treatments, the following are considered:
- Anticonvulsants
- Phototherapy
- Thalidomide
- Systemic retinoids
- Oral steroid
- Tricyclic antidepressant
Prurigo Nodularis Pictures
Collection of photos, images and pictures of the health condition Prurigo Nodularis…
Is Prurigo Nodularis contagious?
Prurigo nodularis is not a contagious disease. It is an inflammatory skin condition with an unknown cause. The condition is believed to be from a repetitive trauma to the skin such as the mechanism of an itch – scratch cycle that resulted in the development of itchy nodules. No harmful pathogens are considered to cause and spread this inflammatory skin condition.