Maculopapular Rash
What is Maculopapular Rash?
This is a skin condition that is characterized by the presence of both papules and macules on your skin which are:
Papules
This is a type skin lesion that are bumps that are one centimeter or smaller in diameter and depending on what caused them they can be brown, pink, red, or purple in color. They do not contain any fluid. They are also usually a symptom of a medical condition and not a medical condition. Heat rash is an example of a papule.
Macules
They are small circumscribed changes in the color of your skin that are neither depressed nor raised nor are they large in size. They are more like a little blemish in your skin and less than a half inch in diameter.
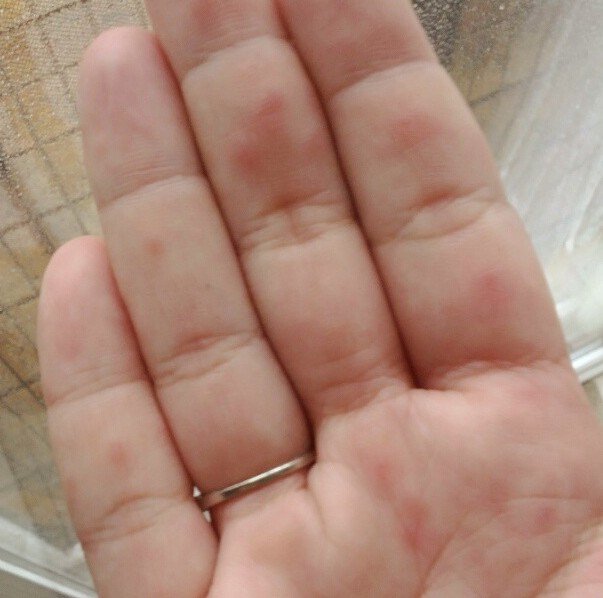
According to the EB Medicine Website, this is the most prevalent type of rash that is treated worldwide in an emergency room. This type of rash has been characterized as morbilliform” by medical experts because maculopapular rash makes a person look as if they have the measles. When a person has maculopapular rash it will usually appear on their face, soles of their feet, trunk, and palms of their hands but it can also appear on other parts of the body.
Maculopapular Rash Symptoms
Usually when a person has a maculopapular rash their skin is usually covered with many little bumps and red. Other symptoms depend on what the cause is.
Measles
In addition to the rash a person will usually have a high fever of one hundred four degrees Fahrenheit. The rash will normally develop a while after having the fever. The colors can change from red to brown before it eventually goes away.
Scarlet Fever
The rash associated with this medical condition will start one to two days after you have the fever and after three to four days it will fade away and the skin will start to peel away in the area affected.
Marburg hemorrhagic fever
The symptoms of this serious medical condition will develop rapidly. The maculopapular rash will develop approximately five days later and in a fourth of all the people who have this hemorrhagic fever will die.
A person may also have severe swelling of their lymph nodes and if it is caused by a severe allergic reaction you could also go into shock and die if not treated. Some may even experience itchiness, have skin that blisters and is painful and warm to the touch.
Maculopapular Rash Causes
Having both of these elements is an indication of a maculopapular rash that is often a part of an acute or serious condition. Some of these medical conditions that can cause a maculopapular rash can include:
- Measles
- Heat rash
- Scarlet fever
- Some hemorrhagic fevers like Marburg hemorrhagic fever or Ebola hemorrhagic fever.
- Having an allergic reaction to amoxicillin, which is an antibiotic and is the main reason that a person will develop a maculopapular rash.
- Medications that are used to ease pain, or treat cancer, or bolster immunity. Some of the medications can include dapsone, phenytoin, or sulfonamides.
- Epstein-Barr virus
- Chikungunya and Dengue – these are two viral diseases that are transmitted by mosquitoes.
- HIV – this appears in some patients with HIV because of the HIV-1 virus and is referred to as an HIV rash.
If the maculopapular rash is spaced randomly around your body it could be caused by many different medical conditions such as hoof-and-mouth disease, Rocky Mountain spotted fever, or syphilis. It is also sometimes seen in people who are undergoing a blood transfusion.
Maculopapular Rash Pictures
Photos, Images and Pictures collection of Maculopapular Rash…
Maculopapular Rash Treatment
Before any type of treatment can be done the physician must determine what is causing you to have a maculopapular rash. If it is because of a serious allergic reaction the physician will narrow it down as to what caused the rash and either remove it from their diet if it is was caused by a food allergy or change their medication if the medicine you were on if that was the cause.
If there is itching along with the rash the treatment may prescribe an antihistamine or have you take an over-the-counter antihistamine. A physician may also prescribe anti-inflammatory medications and antibiotics. You should also make sure that you are drinking plenty of liquids to help flush out any microbial agents that could be causing the infection and to help make sure that you do not become dehydrated.