Lump on Back of Neck
Causes of Lump on Back of Neck
The lump is defined as any protrusion or abnormal enlargement that develops under the skin or above the skin. It is a common occurrence among the general population which at times causes an alarm to the patient for the fear of something else besides being harmless.
The growth of the lump can be so large and evident or it can be so small that it can go unnoticed. Lump can grow in any part of the body including the neck. Most cases of lump growth on back of neck are benign or non-cancerous. In some cases, however, the growth may signify something more serious such as cancer. It is therefore imperative to consult a physician when a lump on back of neck is noticed to determine the extent and seriousness of the condition.
Lump on back of neck for most are often caused by minor conditions although in some cases it can be due to something more serious such as the development of cancer. The location of lump in the neck is significant in determining what the lump is and its cause. The lump at the back of the neck can be alarming but it is usually painless and harmless and which have no impact in the daily activities of an individual.
The development of lump on back of neck can be due to several reasons such as:
Swollen lymph node
Swollen lymph node is among the most common cause of lump on back of neck. The lymph nodes are generally found throughout the body and mostly under the arm and neck. These lymph nodes are an important component of the lymphatic system which is where the waste from filtered bacteria are being stored and eventually destroyed by white blood cells. The lymph nodes can swell when it is filled with too much bacteria and an infection occurred. The swelling can cause the lymph nodes to enlarge and become palpable. Swollen lymph nodes can cause pain and discomfort in and around the neck and can make movement of the neck rather difficult. There are generally a lot of reasons to cause the lymph nodes to swell. Glandular fever is a type of fever that is caused by an infection and can cause swelling of the lymph nodes particularly at the sides and back of neck. Sore throat and common cold can also cause the lymph nodes to swell, resulting in a palpable lump.
Tonsillitis
Tonsillitis is the inflammation of a ball shaped structure located at the back of the throat and is known as tonsil. It can be seen hanging just above the base of the tongue. The major role of tonsil is to protect the body from any bacteria and harmful organisms that may enter the body through the throat. While the tonsil is safeguarding the body from invasion of bacteria and other harmful organisms, it can get inflamed and swell in the process due to an overload of bacteria. When this occurs, a lump will form at the front of the neck and will subsequently form a lump on back of neck as the infection progresses. This will result to a palpable lump on the back of the neck and other symptoms such as difficulty in swallowing, pain and the onset of fever.
Muscle or tendon injury
This is one of the common causes of lump on the back of the neck. The muscle or tendon has basically moved from its original position when it is injured. The injury will result in damages in the muscle, which will later protrude and form a lump, particularly at the back of the neck. When an injury to the muscle or tendon occurs, it will cause a sharp pain, stiffness and difficulty in moving the head.
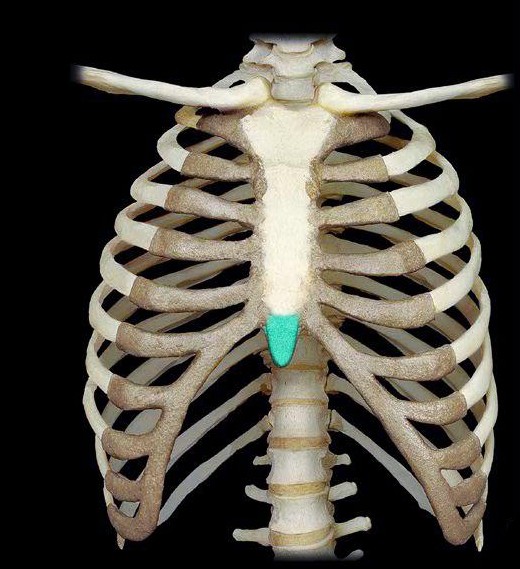
Lymphoma
Lymphoma is one of the serious conditions that can cause the formation of a lump at the back of the neck. Lymphoma is the cancer of the lymphatic system characterized by the uncontrollable proliferation of the white blood cells in the lymph. The rapid and uncontrollable proliferation of the cancerous cells will result it to accumulate and form a mass or lump that can be easily palpated and seen. The accumulation of the cancerous cells and the formation of the hard mass or lump may happen at the back of the neck.
Treatment
The treatment for the lump on the back of the neck depends on the severity and nature of the lump. Most cases of lump on back of neck are benign that treatment is often not necessary although it is still important to consult a doctor for proper evaluation and diagnosis.
The treatment will also depend on what causes the lump to form at the back of the neck. Lump on back of neck that is caused by an infection, for example, can be treated with antibiotics, but swelling of the lymph nodes due to viral infection does not necessitate treatment and usually resolve on its own.
On the other hand, lump on the back of the neck caused by lymphoma is primarily treated by destroying the cancer cells through several treatment methods such as chemotherapy and radiation therapy. Most cases of lump on the back of the neck are benign and the onset usually does not cause discomfort and may not affect the daily activity of life or the quality of life.
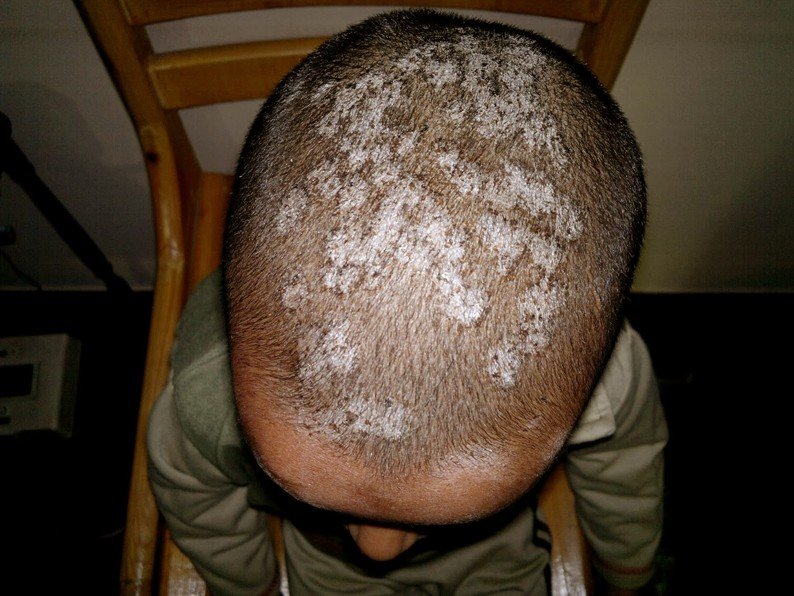
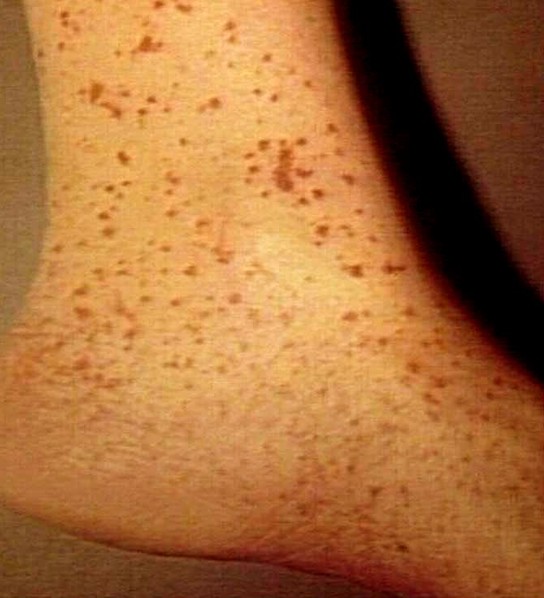
Lump on Back of Neck Pictures
Photos, Images and Pictures of Lump on Back of Neck…