Lichen Nitidus
What is Lichen Nitidus?
Lichen nitidus is a rare, inflammatory skin condition, in which skin-colored, micropapules that glisten appear on the skin. At the moment, it is known that, in this disease, the skin cells present an abnormal inflammatory activity but the exact cause of the inflammation has yet to be identified. Lichen nitidus affects predominantly children and young adults and it rarely causes upsetting symptoms. Once believed to be a variant of lichen planus, now it is found in the medical literature as a skin condition on its own.
Perhaps the most important things that one should understand about lichen nitidus is that the flat-topped papules, be they skin-colored, red or brown, they do not present an increased risk for skin cancer to develop. At the same time, these papules that appear on the skin are not infectious, so you might want to remember that this is not an infectious skin condition. And once a disease is not infectious, it is not contagious either, so you do not have to worry about it being transmitted to another person.
Parents might become frightened when they will see these papules on the skin of their children but it is important to remember this is an inflammatory skin condition. Even though it may look distressing, it is not life-threatening and certainly it does not represent a sign for more serious illnesses.
Lichen Nitidus Symptoms
These are the most common symptoms of lichen nitidus:
- The appearance of small, skin-colored bumps or papules on the skin surface; primarily on the trunk, arms, legs and genital area but they can appear on any skin surface. Keep in mind that the appearance on palms or soles is rare, and so is the one on mucous membranes or fingernails
- If the fingernails are affected, then they may ridge, split or have linear striations on them
- If the inside of the mouth is affected, the the patient might have the following features:
- Flat papules on the inside surface of the cheek
- White plaques on tongue and hard palate
- Papules can heal in a certain surface area and appear on another
- Severe itchiness can appear in rare cases
- Lesions might present an occasional linear pattern or they can gather into clusters, forming plaques
- Tiny blisters or vesicles can appear in rare cases
- Rarely, the pustules can present a central depression
Lichen Nitidus Causes
The exact cause of lichen nitidus has yet to be identified. At the moment, it is known that skin cells present an abnormal inflammatory activity, controlled by the white blood cells that are also known as lymphocytes.
However, there are certain risk factors that the medical literature presents, as lichen nitidus may be associated with the following diseases:
- Lichen planus – as it was already said, at some point, it was believed that lichen nitidus is a variant of lichen planus. However, today, these are two separate entities and it seems that the existence of lichen planus is one of the risk factors involved in the appearance of lichen nitidus
- Atopic dermatitis – this is also an inflammatory skin condition, believed to favor the appearance of the skin-colored micropapules from lichen nitidus
- Crohn’s disease – this is also an inflammatory condition, affecting the interior lining of the digestive tract. As lichen nitidus can affect the mucous membranes from inside the body, you can certainly understand the connection between the two
- Juvenile rheumatoid arthritis – another inflammatory disease, affecting the joints of the body and predisposing to lichen nitidus
- Tuberculosis – infectious disease suppressing the immune system and favoring the appearance of other medical problems, including this inflammatory skin condition
- HIV infection – it has to do with a suppressed immune system as well
- Down syndrome – people with this genetic disorder present an increased risk for various skin conditions, including this one.
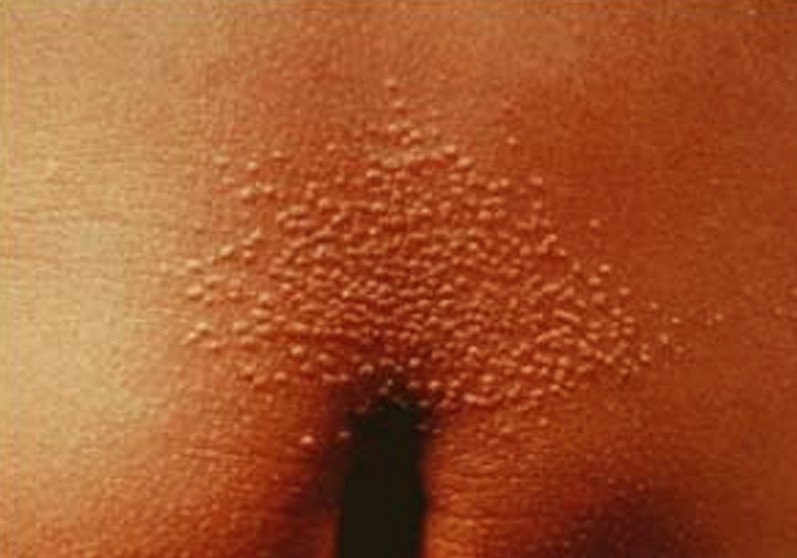
Lichen Nitidus Pictures
Collection of images and pictures of the skin condition Lichen Nitidus…
Treatment
In the majority of the cases, lichen nitidus goes away on its own, without any treatment. There are no scars or changes to the skin color after the lesions have healed. However, there are certain cases in which treatment might be required. These are the most common courses of treatment undertaken by specialized doctors:
- Corticosteroids – these can be administered orally or topically, helping in the reduction of inflammation. However, long term treatments with corticosteroids are not recommended, as they can have serious side-effects and the withdrawal process is quite complicated
- Retinoids – these have the same precaution, as they can irritate the skin and have other serious side-effects as well
- Antihistamines – these are recommended in the situation where there is itchiness reported
- Phototherapy – UVA and UVB light exposure can help with the faster healing of the papules
- Topical calcineurin inhibitors – tacrolimus or pimecrolimus
- Ciclosporins – for more severe cases
- Antibiotics – these are recommended for situations in which there is an underlying infectious condition, such as tuberculosis.
Precautions that you need to take in order to guarantee fast healing:
- Avoid humid and warm environments
- Do not rub the micropapules with a towel when drying off, as this will only contribute to irritating the skin and slowing the actual healing process
- Eliminate sugary foods and wheat from your diet.
Alternative treatments for lichen nitidus include:
- Borax (sodium borate)
- Tea tree oil
- Lavender oil
- Coconut oil
- Comfrey root
- Baking soda
It is important to understand that the natural remedies presented above do not represent a treatment per say for the disease, as this can go away on its own most of the times. They are, however, recommended for patients who are experiencing upsetting symptoms, including inflammation and itching. Plus, it goes without saying that, as opposed to regular medication, these are natural remedies and they do not have any side-effects. They will work strictly on the symptoms you have and bring that much-needed relief you were looking for. Be sure to contact your doctor in case the symptoms do not subside, as you might need medical treatment as well.