Hemosiderin
Definition
Hemosiderin is an insoluble form of tissue storage iron, being found at the level of different cells (not in the circulating blood). This is actually a protein that is insoluble and contains irons, being produced by the digestion of the hematin by the phagocytes. It is a ferritin complex and it is important to understand that the iron that it contains is poorly available for the rest of the body, when it is necessary. The hemosiderin can accumulate in excessive quantities, in the cells of the mononuclear phagocyte system but also at the level of major organs (kidney and liver – epithelial cells).
There are certain medical conditions that can lead to the accumulation of hemosiderin in different tissues, as you will have the opportunity to find out below. While the accumulation of hemosiderin does not cause any obvious symptoms, it is important to note that it will eventually lead to organ damage. Hemosiderin is also found in macrophages and it is believed to be produced in higher quantities, immediately after a hemorrhage has occurred. This has led scientists to believe that hemosiderin might result from the phagocytosis of the red blood cells.
What is the function of hemosiderin?
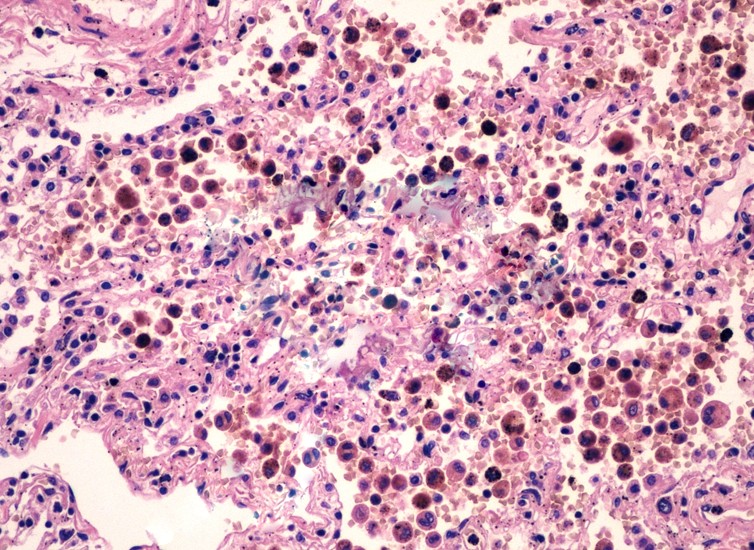 The main function of hemosiderin is to contribute to the repairs that are necessary after an acute hemorrhage. When a blood vessel has ruptured, the red blood cells will die and the hemoglobin (part of the red blood cell) is going to be released into the extracellular space. The reticulo-endothelial system has cells with phagocytic properties; these are also known as macrophages and they will consume the released hemoglobin, leading to the production of biliverdin and hemosiderin.
The main function of hemosiderin is to contribute to the repairs that are necessary after an acute hemorrhage. When a blood vessel has ruptured, the red blood cells will die and the hemoglobin (part of the red blood cell) is going to be released into the extracellular space. The reticulo-endothelial system has cells with phagocytic properties; these are also known as macrophages and they will consume the released hemoglobin, leading to the production of biliverdin and hemosiderin.
Hemosiderin staining
Hemosiderin staining is a medical condition in which one presents yellow or brown patches on the skin. These are in fact the result of the macrophages consuming the dead red blood cells, leading to the production of hemosiderin.
Causes
Hemosiderin staining occurs in patients who have undergone surgical intervention or in those who have suffered from hemorrhage. Those who suffer from cardiac problems also present an increased risk for hemosiderin staining. Patients who suffer from chronic high blood pressure can have such modifications on their skin, due to the breaking of the small blood vessels under the skin.
This modification is encountered in people who have suffered from different types of trauma, whether we are talking about a car accident, blunt force or falling from various heights. The hemosiderin staining can appear as a side-effect of a medical procedure, including after sclerotherapy or regular injections. Systemic health problems, such as venous insufficiency, are known to lead to hemosiderin staining in some patients.
Treatment
These are the most common methods of treatment recommended for hemosiderin staining:
- Topical treatments – cream, ointments, gels
- Vitamin K oxide
- May help eliminate the deposits of hemosiderin
- Available as gel (topical treatment)
- Laser treatment
- Efficient method of treating hemosiderin staining
- May require between one and four sessions of treatment
- The treatment depends on the location of the hemosiderin staining (upper or lower body) and also on other factors: intensity and duration of the staining, skin type
Hemosiderosis (hemosiderin deposition)
Hemosiderosis is a medical condition resulting from the excessive accumulation of hemosiderin in different parts of the body. There are three main types of hemosiderosis, meaning: transfusion hemosiderosis, idiopathic pulmonary hemosiderosis and transfusional diabetes.
These are the most common situations that can lead to the hemosiderin deposition:
- Diffuse alveolar hemorrhage – leads to the accumulation of excessive hemosiderin in the lungs; such modifications can appear in one of the following medical problems:
- Goodpasture’s syndrome – rare autoimmune condition, in which the body’s immune system attacks the lungs and the kidneys (leading to bleeding at the level of the lungs and also to renal insufficiency)
- Granulomatosis with polyangiitis – systemic disorder, in which the patients suffers from both granulomatosis (collection of inflammatory immune cells) and polyangiitis (inflammation of blood vessels, including lymph vessels)
- Idiopathic pulmonary hemosiderosis – lung disease, in which the small capillaries of the lungs become broken and bleed, leading to the excessive accumulation of hemosiderin
- Mitral stenosis – valvular heart disease, in which the mitral valve of the heart becomes narrowed
- Hemochromatosis – iron overload, can be either a genetic disorder or appear as a result of transfusion (especially in the liver, leading to organ failure)
- Diabetes – metabolic disease, in which the levels of blood sugar are constantly elevated
- Chronic subdural hemorrhage – type of hemorrhage that is commonly caused by a traumatic brain injury
- Cerebral arteriovenous malformations – abnormal connection between the arteries and veins at the level of the brain
- Cavernous hemangioma – blood vessel malformation, the dilated blood vessels actually forming a tumor
- Bruising – the color will change as the bruise will heal (hemosiderin being removed from under the skin)
- Stasis dermatitis – medical condition, in which the blood collects in different parts of the body, due to the insufficient venous return
- Paroxysmal nocturnal hemoglobinuria – the immune system attacks the red blood cells, practically destroying them (rare, yet life-threatening disease)
- Conditions that require frequent blood transfusions
- Sickle cell anemia – type of anemia, in which the hemoglobin presents structural abnormalities
- Thalassemia – type of anemia, in which the formation of hemoglobin is abnormal (autosomal recessive blood disorder)
Treatment
These are the most common measures chosen for the treatment of hemosiderosis:
- Phlebotomy
- Immunosuppression
- Limiting the transfusions of blood
- Iron chelation therapy
- In case of pulmonary hemorrhage:
- Oxygen therapy
- Blood transfusions
- Supportive respiratory therapy
- Mechanical ventilatory support
- Immunosuppressive therapy
- Avoidance of milk and dairy products
- Gluten-free diet (for patients who suffer from both hemosiderosis and celiac disease)
- Corticosteroids
- Management of the acute alveolar hemorrhage stage
- Cannot be administered on a long-term basis, due to the wide-range of side-effects
In conclusion, hemosiderin plays a very important part in the human body but it can also cause health problems, when accumulated in excess. In the majority of the cases, the excess accumulation of hemosiderin is a sign of an underlying condition. The diagnosis of hemosiderosis can guide the doctor in discovering the underlying medical problem.