Diabetic Retinopathy
What is Diabetic Retinopathy?
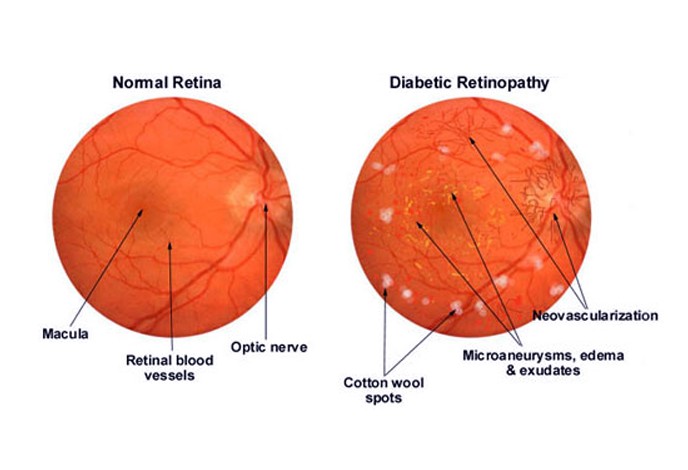
Diabetic Retinopathy is a chronic and progressive disease of the retinal microvasculature as a result of complication from Diabetes. It is a common complication and manifestation of prolonged diabetes or for those patients suffering from Diabetes for more than 10 years.
Diabetic retinopathy is characterized by damage in the blood vessel of the retina or the light sensitive tissue found at the rear of the eye. It is regarded as the leading cause of blindness among people 27 to 74 years of age and is commonly associated with diabetes type 1 and type 2. Patients suffering from long-term diabetes are especially at high risk for diabetic retinopathy.
In type 1 diabetes the onset of diabetic retina is mild and is usually recognized in the 7th year on the average from the onset of diabetes. Type 2 diabetes is the more common type of diabetes where the onset is rather gradual in which the retinal changes may have taken place right before the diagnosis of diabetes.
Diabetes is a metabolic disease described with high levels of blood glucose as a consequence of the inability of the pancreas to produce sufficient amount of insulin in the body or as a result of dysfunction of the pancreas. This metabolic disease is divided into two main types known as diabetes mellitus type 1 and diabetes type 2. Type 1 of diabetes mellitus is also known as juvenile onset diabetes and formerly known as insulin dependent diabetes. It is an autoimmune disease where the pancreas is mistakenly being attacked by the autoimmunity itself leading the pancreas to the inability to produce insulin. Type 2 diabetes on the other hand is known as adult onset diabetes mellitus or the non-insulin dependent diabetes. This type of diabetes is characterized by an overproduction of insulin by the pancreas and is also characterized by the insensitivity of the muscle cells and fat of the body. People over the age of 30 years are at risk for developing diabetes type 2 and the risk increases as the age is also increasing. Diabetes type 2 is commonly associated with obesity where it is found that people who are overweight are at greater risk for developing diabetes.
Diabetic Retinopathy Symptoms
The onset of diabetic retinopathy usually goes unnoticed especially in the early stage of the retinopathy. It is rare for the early stage of diabetic retinopathy to have any symptoms although the progression of the condition may lead to the onset of symptoms. The symptoms on the other hand depend on the stage in which the retinopathy has progressed and with the onset of the symptoms in a gradual manner.
Minimal changes in eyesight may be noticed although most patients still have the normal eyesight despite the onset of retinopathy. Diabetic retinopathy generally affects both eyes and the signs and symptoms are dependent on the stage in which the retinopathy has progressed. Common signs and symptoms on the other if retinopathy has progressed and manifested include the following:
- Gradual reduction of central vision which is usually associated with the formation of cataract.
- Floaters in vision are usually the result of hemorrhages.
- Although painless, severe hemorrhages may lead to loss of vision.
Other symptoms of diabetic retinopathy characterized by changes in vision include the following:
- Double vision
- Blurry vision
- Vision of spots
- Loss of night vision
- Acute pain in the eye may also be experienced which is usually due to the acute attack of glaucoma that is hastened by rubeosis iridis.
- Color perception may also have difficulty as a manifestation of diabetic retinopathy.
- Fluctuation of vision may also occur.
Permanent blindness and retinal detachment usually occur as a complication of diabetic retinopathy during the later stage of the condition.
Causes of Diabetic Retinopathy
Diabetic retinopathy occurs when there is a high level of glucose or sugar in the blood. The tiny blood vessels that supply the retina is thereby damaged by the high levels of blood sugar or may completely obstruct the tiny blood vessels. The damages and obstructions in the tiny blood vessels later result to the retina being cut off with the blood supply.
Insufficient blood supply or in the absence of blood supply in the tiny blood vessels that nourish the retina, changes in vision or a vision loss occur as a response of the retina to the insufficiency or absence of the blood supply. New blood vessels are being formed as an attempt of the eye to improve blood circulation. The attempt however resulted in abnormal formation of tiny blood vessels which are rather fragile and can leak and cause obstruction in the retina or at the back of the eye.
The obstruction of the retina is the result of the swelling that occurred during the course of fluid leakage into the macula. The swelling of the macula directly affects the color perception and the ability to see minute details resulting to changes in vision particularly a blurry vision.
The lenses of the eyes can also get affected by the high levels of blood sugar. Long period of high blood glucose can later cause the lenses to swell thereby resulting to changes in vision or a blurry vision. Formation of scar is also another concern which can later pull on the retina causing a retinal detachment.
People with long-term diabetes are at high risk for developing diabetic retinopathy. A blood sugar that is not managed properly or improperly controlled can put an affected individual at risk for diabetic retinopathy as well. Pregnant women who later developed gestational diabetes are also at risk for diabetic retinopathy as they increase in age. Other medical conditions such as elevated blood pressure and increased blood cholesterol can also put one at risk for developing diabetic retinopathy overtime.
Stages
Diabetic retinopathy is classified into two types which described the stage of retinopathy among patients. The two stages of diabetic retinopathy are as follows:
Non-proliferative diabetic retinopathy
This is the early stage of retinopathy. It is characterized by mild and non-existence of symptoms. This stage of retinopathy has no significant formation of new tiny blood vessels that are rather abnormal and formed improperly. Microaneurysm or the protrusion of the tiny bulges in the weakened walls of the blood vessels of the retina may occur during the early stage of retinopathy. The protrusion can cause fluid and blood leakage into the retina and may have the tiny blood vessels obstructed as the condition progresses. The obstruction and the swelling can affect the retina or the lenses of the eyes that leads to the changes in vision or the blurry vision.
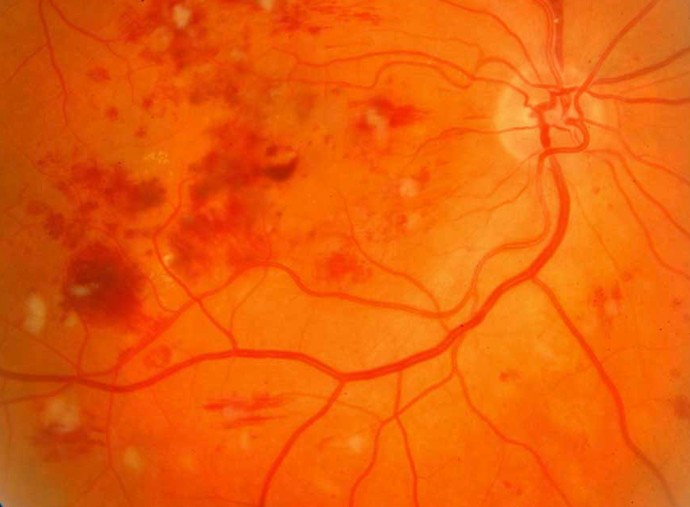
Proliferative diabetic retinopathy
This is the advance stage and the most severe form of diabetic retinopathy. This stage is marked by the formation of new tiny blood vessels that are abnormal and improperly formed. The retina during this stage is already deprived with oxygen supply which triggered the eye to form the tiny blood vessels in an attempt to sufficiently supply the eye with oxygen.
Diagnosis
Dilating the eyes is the initial step in diagnosing diabetic retinopathy among patient preceded by medical history taking. During the exam the eyes of the patients are dilated and an eye doctor takes note of the presence or the absence of the cataract that could possibly be causing the changes in vision. Formation of new and abnormal blood vessels are being evaluated including the swelling and deposits of fats and blood in the retina. Other abnormalities formed such as scar formation, retinal detachment and bleeding are also evaluated during the examination.
Additional tests may be done to confirm diabetic retinopathy and such tests include the following:
- Measurement of visual acuity
- Measurement of pressure
- Optical coherence tomography
- Fluorescein angiography
Diabetic Retinopathy Treatment
The treatment for diabetic retinopathy depends on the stage of the retinopathy including its extent. Non-proliferative diabetic retinopathy or the early stage of retinopathy usually require no treatment but close monitoring is required to evaluate for progression of the condition and if treatment will then be warranted.
Proliferative diabetic retinopathy is the most severe type of retinopathy that requires surgery. Surgical procedures however depend on the problems in the retina that occurred.
Laser photocoagulation is a procedure utilized to impede the fluid leakage or blood leakage into the retina. The leaks are being sealed with the laser beam which burns to seal the tiny blood vessels causing the leakage.
Panretinal photocoagulation is another method used to treat proliferative diabetic retinopathy that has caused widespread growth of blood vessels into the retina. Saving the central vision is the goal of this procedure and some vision on the peripheral on the other hand may be lost after the procedure.
Vitrectomy is a procedure utilized to remove the blood vessels that formed in the vitreous and other areas of the retina. Scar tissues and tiny blood vessels that formed in the retina are being removed with the use of delicate instruments while salt solution is being placed to maintain the shape of the eye.