Dents in Fingernails
The dents in the fingernails can cause a lot of embarrassment, especially when you are at work or out on the town, with friends. Apart from embarrassment, there are a lot of people who are conscious that this might be a sign of a medical condition. They seek out medical treatment and learn the exact cause. The doctor can also recommend methods of prevention for such problems. The important thing is that you do not waste time in seeking out the correct treatment. By taking the correct treatment, soon you will have healthy and beautiful fingernails again.
What Causes Dents in Fingernails?
These are the most common causes that lead to the appearance of dents in fingernails:
- Psoriasis
- Psoriatic nails have a specific aspect
- The fingernails present dents, plus they are discolored or pitted
- May have modifications under the nail plate as well
- Reiter syndrome
- Reactive arthritis
- Occurs after a bacterial infection
- Modification of the fingernails – dents
- Alopecia areata
- The production of keratin is affected, leading to hair loss
- The dents in the fingernails can appear at the same time with the hair loss or as an after-process
- Fingernails are made from keratin as well, so it is understandable why alopecia areata will lead to such modifications
- Incontinentia pigmenti
- Genetic disorder (gene mutation)
- Hyperpigmentation of the skin
- Dents in the fingernails
- Dental modifications
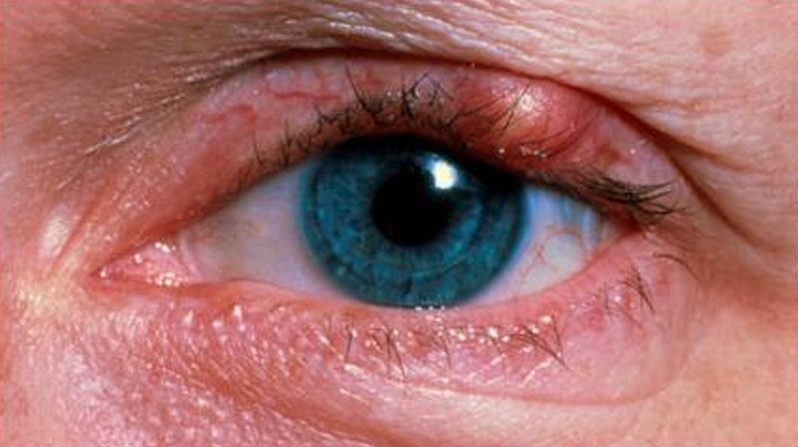
- Eye problems
- Vitamin deficiency
- When dents appear in the fingernails, they can be a sign that the body lacks vitamins, such as the ones from the B complex (B12 or B6 in particular)
- Iron deficiency can also cause dents in the fingernails
- Nail trauma/injury
- Direct accident
- Frequent biting of the nails
- Fungal infection
- Can lead to dents in the fingernails, among other modifications
- Thyroid problems
- Hormonal imbalances can lead to modifications in the fingernails, dents included
- Medication
- Dents in the fingernails can appear as a side-effect of medication
- Stress
- Excessive stress can lead to modifications in all parts of the body, including the fingernails, causing dents to form
- Cyst
- Often appears in arthritis patients
- The fingernails present deep dents, with the cyst being present at the end joint of the finger, right in the near vicinity of the nail
- If the cyst subsides, so will the dents in the fingernails
- Diabetes
- Can lead to dents in the fingernails
- Cancer
- The modifications in the fingernails appear in patients who have been treated for cancer (chemotherapy)
- Raynaud’s phenomenon
- The dents in the fingernails appear after periods of long exposure to extremely cold temperatures
- Circulatory problems
- They can affect the health of the fingernails, causing dents to appear, among other modifications.
Treatment for Dents in fingernails
 In order for these modifications to be improved, the underlying conditions must be treated first:
In order for these modifications to be improved, the underlying conditions must be treated first:
- Psoriasis
- Corticosteroid cream
- Salicylic acid cream
- Synthetic vitamin D cream
- Avoidance of triggering factors
- Change of diet
- Reiter syndrome
- Antibiotics to prevent secondary infections
- Medication to suppress the response of the immune system
- Anti-inflammatory medication – pain relief
- Corticosteroids – cannot be administered as long-term treatment
- TNF (tumor necrosis factor) inhibitors
- Alopecia areata
- Corticosteroids – administered as injections
- Topical creams with corticosteroids
- Topical immunotherapy
- Ultraviolet light therapy
- Incontinentia pigmenti
- Topical tacrolimus
- Topical corticosteroids
- Skin moisturizers
- Antibiotics to prevent secondary infections
- Vitamin deficiency
- Administration of vitamin supplements
- Diet changes
- Nail trauma/injury
- Immediate medical care for nail trauma
- Excellent nail hygiene during recovery
- Avoidance of nail biting
- Fungal infection
- Topical ointments or cream with anti-fungal properties
- Oral medication is recommended in more severe cases, with no response to topical treatments
- Thyroid problems
- Administration of thyroid hormones to restore hormonal balance
- Medication
- Change of medication (new alternative – no side effects)
- Stress
- Relaxation techniques
- Breathing exercises
- Psychological counseling
- Cyst
- Rheumatic treatment – allows for the cyst to subside and the nail health to improve
- Diabetes
- Medication to keep the condition under control
- Adapted diet
- Cancer
- Change of chemotherapy medication
- Pause between chemotherapy sessions
- Raynaud’s phenomenon
- Avoidance of exposure to cold temperatures
- Massage and electrotherapy
- Circulatory problems
- Medication to stimulate the blood flow
- Active physical exercises – adapted to the existent problems
- Warm baths to improve blood circulation
- Avoidance of exposure to cold temperatures
- Medication to prevent the blood from becoming either too thick/thin.
How to Prevent Dents in fingernails
If you are interested in preventing the appearance of dents in the fingernails, this is what you should do:
- Consider taking vitamin supplements
- Do not wait until the fingernails present modifications
- Go to the doctor and have yourself tested for vitamin deficiency
- Taking vitamin supplements can prevent the appearance of dents in the fingernails
- Eat a healthy diet
- Your diet should contain plenty of fresh fruits and vegetables, as these contain a lot of vitamins and nutrients
- Look after your fingernails
- Avoid keeping them for prolonged periods into water
- Keep them trim and clean, to avoid infection
- Do not bite your nails
- Don’t cut your cuticles too short
- Don’t use your fingernails to open things
- Wear protective gloves if you need to work with harsh chemicals
- Use a delicate hand lotion to keep the fingernails moisturized
As you can see for yourself, when it comes to dents in the fingernails, one must treat the underlying condition first. As for the methods of prevention, this can ensure that such problems will not bother you. By looking after your fingernails, you will make sure that you are protected against infection and other problems like that. Also, eating healthy is a must, as fingernails need vitamins in order to remain healthy. A very useful tip is to drink plenty of water: if you drink the recommended quantity each day, then the fingernails are going to look and be healthy, without any dents.