Lentigo Maligna
What is Lentigo Maligna?
This is a skin condition, also known as Hutchinson’s melanotic freckle or melanoma in situ. Basically, in parts of the skin that were damaged by the sun, these malignant cells appear without any invasive growth. The progression of the skin condition is very slow and it may remain in the non-invasive form for years.
Lentigo maligna is commonly encountered in people who have entered their 9th decade, the most affected areas being the ones that received constant sun exposure, such as the face (especially nose and cheeks) and the forearms. In this form, the malignant cells are confined to the initial tissue and their growth is slow but it can be make the transition to genuine melanoma. That is known as lentigo maligna melanoma and it is characterized by the malignant cells transforming into bumpy surfaces.
What does lentigo maligna look like?
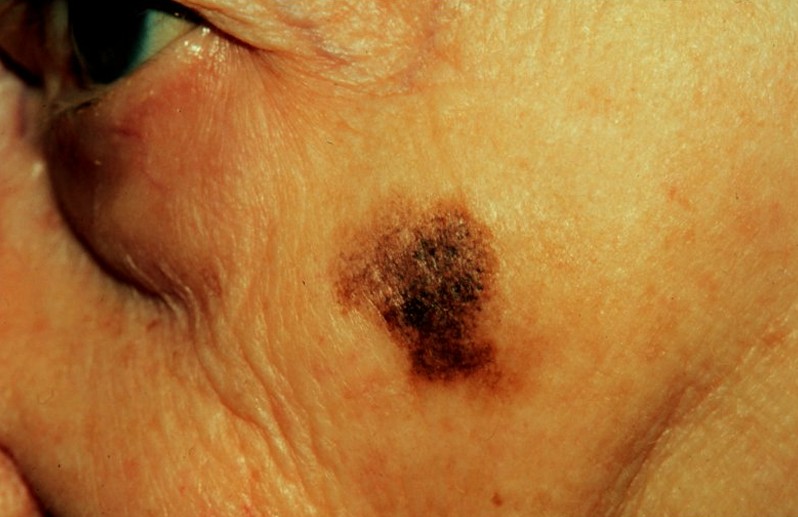
Initially, blue or black stains appear on the skin. As this condition appears in the elderly, it should come as no surprise that the skin is thin. In many patients, the skin becomes discolored in certain areas and this areas expand slowly with the passing of time. The resemblances in the initial period is of freckles or brown spots, also known as lentigines. The affected areas become more obvious in time, having the possibility to grow to even as several centimeters over the course of decades.
In order to recognize lentigo maligna, one has to follow what is known as the ABCDE rule. A stands for asymmetry, B for irregularity of the border, C for variation of color, D for large diameter and E for evolving. According to this rule, lentigo maligna has a large size, an irregular border, color variation (brown, blue, pink, red or white) and a smooth surface to the touch (this is because the skin becomes thinner due to aging).
Symptoms of Lentigo Maligna
These are the most common symptoms of lentigo maligna:
- Discolored skin surfaces that may expand with the passing of time
- Growths on sun-exposed skin – nose, cheeks, ears, neck, forearms
- Tingling or itching can occur
- If the skin is hard and lumpy to the touch, bleeding, oozing or crusting, then it has probably already migrated to lentigo maligna melanoma
Causes
The exact cause why the skin cells become malignant has yet to be identified but it seems that a genetic mutation might be involved.
Prolonged and constant sun exposure is the main trigger factor incriminated, especially during the young years of one’s life. This is the reason why having a fair skin and living in a country where there are lots of sunny days become two other potential triggering factors. It goes without saying that the constant exposure to sources of artificial tanning can increase the risk for lentigo melanoma to appear as well.
Having a fair skin is a potential risk because this is the type of skin that is easily damaged by the sun. These are the people who rather burn than tan, having light-colored hair (blonde or red) and light-colored eyes (blue or green). They also have freckles and, as it was already mentioned, lentigo melanoma is also known as the melanotic freckle. It goes without saying that this is a skin condition less common in people with darker skins.
As sun exposure is considered to be the main triggering factor, it seems that having periodic severe sunburn episodes is also a favoring factor. If those episodes took place during childhood and they were severe enough for blisters to form on the skin, then that skin was already hurt and predisposed to lentigo melanoma in older years. Last, but not the least, it seems that people with numerous moles on their bodies and especially hairy birthmarks present an increased risk for this skin condition, as there are those who suffer from immune-deficiency.
Diagnosis
The ABDCE rule is often used for the diagnosis of lentigo melanoma but this is only related to the initial assessment. Often time, a specialist doctor will prefer to see the affected tissue under a microscope. The whole area will be removed surgically and then it will be sent to a specialized laboratory for further examination. In cases of areas that have grown too extensively, then only a sample will be taken, which is known as a biopsy. This is extremely important, as it can determine whether the malignant cells have breached the border and what course of treatment should be taken.
In most of the situations, the surgical removal of the entire affected area is contraindicated, as the initial identity of the lesion cannot be so easily pinpointed. The type of biopsy performed is then the one where the doctor will take samples from multiple points. The samples taken might show different things and it will help the doctor to locate the initial identity of the lesion, thus being able to excise it completely.
Prognosis
First of all, you should understand that lentigo maligna is not dangerous, as it evolves slowly over the years but the malignant cells stay within a certain border. However, if they make a turn for melanoma, then the prognosis changes. The prognosis depends on whether the lesions can be removed surgically or not, the efficiency of other treatments and also on the appearance of new, modified lesions. The moment the diagnosis of lentigo maligna melanoma has been made, the prognosis depends on the thickness of the tumor.
Treatment
These are the most common courses of treatment for lentigo maligna:
- Surgical removal of affected area, followed by additional skin grafting
- In cases where the surgery cannot be performed because the affected area is too large, there are other treatment options available:
- Radiotherapy
- Cryotherapy
- Topical creams – the results of these creams are still in the research phase.
When it comes to having lentigo maligna, prevention is the key, in order to prevent it from becoming lentigo maligna melanoma. These are a few key recommendations:
- Go to the doctor the moment a mole has changed its form, color, growth or if it has started to bleed or ooze.
- Protect yourself from the sun using creams with high SPF factors and wearing appropriate clothing during hot summer days.
Do not use artificial tanning.
Survival rate
The survival rate for lentigo maligna is normal, as this is a slowly progressing disease. Co-existing factors might affect the rate of survival, especially if the patient will have to undergo prolonged surgery for extensive removal of the affected area. In the situation that lentigo maligna turns into a melanoma, then the survival rate for those over 4 mm is of 50% during a period of ten years.
Once again, the survival rate depends on how the lesions have spread and whether they have suffered modifications. The survival rate can be definitely influenced by the overall health of the patient, as it a well know fact that older patients can have various chronic medical problems.
As a patient, you should not wait to go to the doctor until it is too late. The treatment and the survival rate are both influenced by the actual time when you go to the doctor, as the progression from lentigo maligna to melanoma can happen without any notice.
Lentigo Maligna Pictures
Collection of pics, photos and pictures of the skin condition Lentigo Maligna…