Akathisia
Do you have a feeling to keep moving at all times? Or have your friends been telling you that you are abnormally in motion? A feeling of the compulsion to be in motion at all times or a feeling of inner restlessness exists in some people, though the percentage of persons who have this condition is low.
If you have noticed it yourself or some other persons have complained about what they are noticing concerning your restlessness, it is possible that you may be suffering from a medical condition known as Akathisia. The awareness of this problem should not make you further restless as there are potent treatments for it. You can be treated and all the symptoms go away to enable you resume your normal life again.
In this post, we shall take a look at what Akathisia is, its signs and symptoms, the causes, diagnosis, and treatment. So, if you have the challenge or know of someone who has it, relax and get some useful information from this post because they will definitely be of immense help to you.
What is Akathisia?
Akathisia is a disorder of movement which is distinguished by a feeling of impatience and a kind of pressure to continually move around. It is also characterized by actions like lifting the feet as if doing an on-the-spot marching, crossing the legs or and uncrossing them while in a sitting position, as well as swinging while sitting or standing.
Akathisia sufferers find it almost impossible to keep or sit still, and they are usually pacing, fidgeting, rocking from foot to foot, and constantly restless.
Symptoms of Akathisia
Some of the symptoms of akathisia include the following:
- Anxiety
- Painful discomfort especially in the knees
- Swaying or rocking from foot to foot
- A sense of inner discomfort or tension or a sense of needing to move
- Twisting
- Poor posture
- Muscle kinks
- Shifting repeatedly
- Twisting of the trunk or waist
- Repeatedly crossing and uncrossing the legs
- Lifting the feet as if marching
- Difficulty standing without pacing or walking
- Repeated bending of the neck or nodding of the head.
Causes
Akathisia is caused mainly by drugs, hence it is referred to as a drug-induced condition. However, it must be understood that the condition is not caused by just one type of drug. Below are a few known drugs that bring about akathisia.
Antipsychotics/Antidepressants
Akathisia has been found to result from a reduction in the level of dopamine signals in the brain. Besides, it is also caused by a rise in the level of serotonin signals. This makes akathisia to show up as a side effect of antidepressant or antipsychotic medications, or during the period of withdrawing from the use of the drugs.
Anti-migraine or anti-nausea medications
Some drugs used in the management of migraine or nausea also act like the aforementioned drugs and so, they are able to cause akathisia, though this is not common. The period between the use of the medication and the appearance of akathisia differ in people. While the condition shows up shortly after the commencement of the medication in some persons, it takes some months for it to manifest in others.
Selective serotonin reuptake inhibitors (SSRIs)
This is not purely a cause, but an existing akathisia is known to be exacerbated by SSRIs.
Drug withdrawal (barbiturates, cocaine, opioids or benzodiazepines)
Symptoms can manifest in a matter of weeks if the condition is a result of drug withdrawal. It is therefore, important to watch out for symptoms of akathisia weeks after withdrawing from opioids or any other stimulant drugs.
Other drugs
Research has shown that the above-listed groups of drugs are not the only ones that contribute to the development of akathisia. Some other drugs that have been implicated include Levodopa, methyldopa and dopamine antagonists, anticonvulsants, interferon alfa, lithium carbonate, sumatriptan, buspirone, pethidine, etc.
Diagnosis
Akathisia can be diagnosed using the Barnes Akathisia Scale. This scale is used for measuring the presence or severity of the condition. It assesses both subjective and objective criteria. It is difficult to accurately assess akathisia because a lot of disorders with similar symptoms are hard to differentiate. The main features that differentiate akathisia from other syndromes are primarily characteristics that are mostly subjective, such as a sense of impatience.
Treatment of Akathisia
Care must be taken when treating akathisia. Because it is usually induced by drug, treatment would require stopping the drug, reducing the dosage used for an existing treatment, or adopting a new drug. However, if you are currently on an antidepressant or an antipsychotic medication, it must have been prescribed for a reason. So, readjusting drug dosage may lead to untoward effects or even cause a further relapse in the psychiatric condition being treated with the drugs.
It would be wise to see your doctor if you notice that you have akathisia. The doctor knows exactly the type of medication to prescribe for you and how to handle the dosage in the course of managing the problem. However, here are some of the things the doctor is likely to recommend for you.
Dose adjustment
The symptoms can be controlled by adjustment in the dosage of the drugs. This must be purely managed by a professional doctor who would be sure that the reduction in dosage is achieving its intended purpose. However, if you are managing akathisia caused by benzodiazepine or opioids withdrawal, the reverse is usually the best – increasing the dosage temporarily and then gradually reducing it over certain periods may produce a significant improvement in the symptoms. Neuroleptic drugs should not be withdrawn abruptly lest they cause further problems.
Drug holidays
Sometimes, your doctor may advise you to go off the drug for a certain period to see if this can help alleviate the symptoms. You can even suggest to the doctor to allow you go on holidays while you watch the symptoms. But you should never stop the drugs on your own without consulting your doctor.
Change in prescription
It is possible for second-generation antipsychotic and antidepressants to still cause the condition. But they do this much more slowly than when the other drugs are employed. Find out from your doctor if it is possible to use alternative drugs.
Anticholinergics
Anticholinergics help in blocking some neurotransmitters. They are quite useful in some cases of akathisia, though they are primarily used in the management of respiratory, sleep-related or digestive conditions. Anticholinergics produce some funny side effects; it is better to try other medications before deciding to use them.
GABA Analogues
If the akathisia is caused by withdrawal from opioids and it is no longer possible to continue on the opioids, then GABA analogues like gabapentin and pregabalin which are generally used for the management of acute idiopathic akathisia may be used in some cases.
Other drugs
Neuroleptic-induced akathisia is also known to respond to certain drugs like β-adrenergic antagonists (e.g. Propranolol), serotonin antagonists (e.g. cyproheptadine), and Benzodiazepines (e.g. lorazepam). They can be helpful as alternative treatments for the condition.
Change of diet
Some of the symptoms of akathisia respond positively to Vitamin B6. Since the vitamin assists in reducing the symptoms, you should try and eat foods rich in Vitamin B6. Such foods include meat (such as beef and turkey) and carbohydrates like potatoes.
Is Akathisia permanent?
The answer to this question is a two-way thing. Akathisia can be both temporary and permanent conditions. If it is caused by medications, the withdrawal, reduction in dose or the switching of such drugs should normally bring an end to the condition. This depends on how well the drug issue is handled. Withdrawing some drugs like cocaine or opioids can worsen the condition.
However, it should be noted that some forms of akathisia can still continue for years even when you have stopped using the drugs that initially caused the problem. So, akathisia could go away when the cause is identified and removed early enough. But if it not handled on time, it can become a permanent condition.
How long does Akathisia last?
Akathisia can last for less than 6 months or it can also last for several years. When it lasts for less than 6 months, the condition is referred to as Acute Akathisia. But when it lasts for more than 6 months into several years, it is known as a Chronic Akathisia. Acute akathisia responds to treatment and goes away within six months. The chronic type is difficult to handle and it is generally slower in responding to treatment. In a nutshell, akathisia lasts from less than 6 months to several years, depending on the cause and how it is handled.
Conclusion
You should never take drugs that are not prescribed by your doctor. If you are on any medication and notice any strange development in your mood or movement, see the doctor immediately. It is always better to start handling Akathisia in the early stage because the prognosis is usually better when treatments are commenced on time.
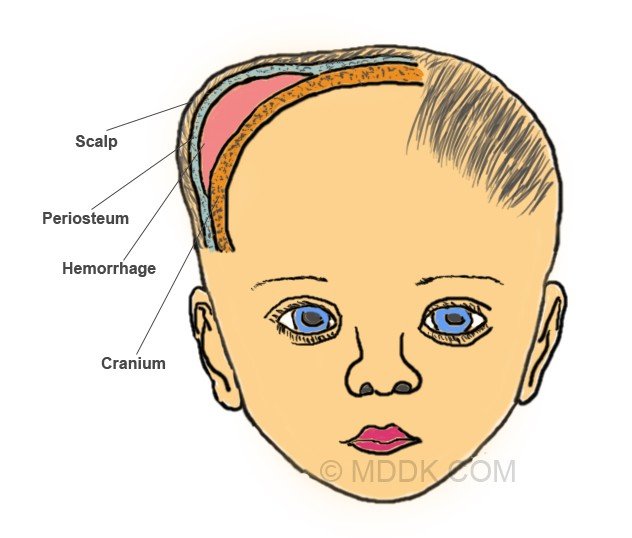
 Cephalohematoma Picture 2 (Top of Baby’s head) : Cephalhematoma, Galea aponeurotica, Scalp, Subgaleal hemorrhage, Skull and periosteum, Dura mater, Arachnoid membrane, Sudural hematoma and Epidural Hemorrhage
Cephalohematoma Picture 2 (Top of Baby’s head) : Cephalhematoma, Galea aponeurotica, Scalp, Subgaleal hemorrhage, Skull and periosteum, Dura mater, Arachnoid membrane, Sudural hematoma and Epidural Hemorrhage