Central Pontine Myelinolysis
Central pontine myelinolysis can be defined as a medical condition, in which the myelin sheath of the nerve cells in the brainstem become severely damaged. This is a neurological disease, with a specific location (area known as the pons) and iatrogenic etiology. Also known as osmotic demyelination syndrome or central pontine demyelination, this condition can lead to a wide range of symptoms. As you will have the opportunity to read below, one can suffer from acute paralysis, present difficulties swallowing and speaking. In some patients, the condition can appear outside the mentioned area.
This condition appears in the majority of cases as a complication to the treatment of patients who present life-threatening, low levels of sodium in the body. In order to prevent the appearance of this condition, one should correct these levels in a gradual manner (specific rate of sodium to be administered on a daily basis). There are other situations that may lead to central pontine myelinolysis, even though they are less common. Chronic alcoholism and the reduced functioning of the liver have been incriminated among the causes.
This condition was described for the first time in the 1950s, being observed in those who suffered from chronic alcoholism or malnutrition. As the studies extended, it was recognized that the primary cause was the too rapid correction of sodium levels in those who suffered from hyponatremia. In was only in the 1980s that the condition was established, with the guidelines we know today. Both adults and children are at risk of developing this condition, especially if there is a rapid rise in the serum sodium levels. It is important to understand that this condition never occurs on its own – as it was already mentioned, it appears as a complication of other medical problems or treatments.
Pathophysiology
The osmotic concentration is adjusted by the brain cells, with the levels of certain osmolytes being changed on a regular basis. When the sodium levels are dangerously low, the levels of the osmolytes are also affected and so is the capacity of absorbing free water. If the correction of sodium levels is too rapid, this means that the free water will also leave the brain cells. It is this change that leads to the appearance of central pontine myelinolysis, with paralysis and other neurological symptoms. Due to the lack of water, the brain appears as if it would shrink.
As the nerve fibers at the level of the brain suffer from demyelination, damage occurs. If the levels of sodium are chronically low, the brain can adapt to these changes and compensate by taking water from the interstitial area. On the other hand, if the correction of sodium is made with intravenous fluids, the brain might not have sufficient time to adapt to the changes. Basically, the more rapid the correction is made, the more water the brain will lose and suffer from additional damage. The damage is caused by the appearance of cerebral hemorrhage, which is a consequence of water moving into the cells.
Causes
These are the most common causes that lead to the appearance of central pontine myelinolysis:
- Trying to correct the life-threatening low sodium levels too rapidly
- Chronic alcoholism (especially in patients who are suffering from withdrawal symptoms)
- In patients who have undergone hematopoietic stem cell transplantation
- Reduced functioning of the liver due to severe disease
- Transplantation of the liver
- Patients who have suffered from severe burns
- Eating disorders (malnutrition, anorexia, bulimia)
- Severe disorders of the electrolytes
- Excessive or prolonged usage of diuretics
- AIDS
- Hyperemesis gravidarum – rare complication of pregnancy
- Peritoneal dialysis, leading to reduced sodium levels
- Wernicke encephalopathy
- Diabetes (very rare).
Diagnosis
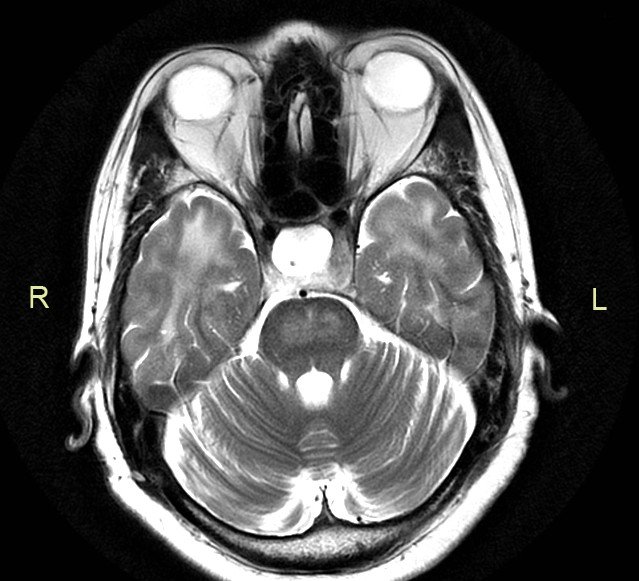
Central pontine myelinolysis is difficult to diagnose using imaging studies. In the majority of the patients, the changes take several weeks after the onset of the symptoms before they appear visible on the MRI or CT. In general, the MRI is more recommended than the CT, due to higher fidelity of the investigation.
The physical examination can also reveal changes related to this condition, such as: abnormal reflexes, confusion, weakness or paralysis. Apart from the head MRI scan, the doctor can also order blood tests (sodium levels) and perform the brainstem auditory evoked response (not as faithful as the MRI). For the latter, electrodes are attached to the head and ears; then, a series of sounds are played through the headphones. The investigation determines the activity of the brain in response to those sounds.
Symptoms
These are the most common symptoms associated with central pontine myelinolysis:
Precursor symptoms
- Seizures
- Affectation of consciousness
- Changes in the gait
- Affectation of the respiratory function (decreased/ceased)
Acute symptoms
- Paralysis (can affect two or all of the limbs)
- Difficulties swallowing (dysphagia) and speaking (dysarthria)
- Problems with the vision (diplopia)
- Loss of consciousness
- Confusion and delirium
- Balance problems (unstable gait)
- Hallucinations
- Lethargy
- Poor response
- Tremors
- Weakness in different parts of the body
Locked-in syndrome
- Cognitive function is intact
- All muscles are paralyzed (exception – eye blinking)
- This syndrome appears in the situation that the corticobulbar and corticospinal tracts of the brainstem have suffered from rapid myelinolysis.
In some patients, this condition does not present any symptoms, which is suggestive of the fact that the lesion in the respective area of the brain is not that big. The symptoms mentioned above appear in patients who have suffered from bigger lesions.
Prevention and Treatment
The most certain way to prevent central pontine myelinolysis is to correct the reduced sodium levels in a gradual manner. If these are corrected at a slow pace, the risk of overcompensation is reduced and the brain has the necessary time to adjust to the changes. In case of patients who suffer from chronic alcoholism, vitamin supplementation can help prevent such problems.
Unfortunately, once central pontine myelinolysis has occurred, there is no cure. Patients can benefit from supportive care, with the main objective being the prevention of life-threatening complications, such as aspiration pneumonia or deep vein thrombosis. Vitamins can be administered to those who suffer from chronic alcoholism, so as to correct the other nutritional deficiencies. Corticosteroids have been used as a line of treatment (experimental phase) but their efficiency has proved out to be reduced.
Physical therapy and rehabilitation are essential during the recovery phase, as they can contribute to the overall improvement of the prognosis. The physical therapist can help with the reduction of spasticity, while working to maintain the strength and force of the muscles. As the patient recovers, the physical therapist will add exercises to increase mobility and function. The patient will be taught transfers to/from bed and to/from chair, learning how to sit and stand without getting dizzy. The last phase of the recovery process is going to concentrate on the improvement of the balance and walking (on his/her own or using assistive devices). Speech therapy is recommended to those who have trouble speaking and occupational therapy is essential for the daily living activities. The occupational therapist can teach the patient how to function on a daily basis, maintaining the highest level of independence that is possible.
In the situation that the patient has developed Parkinsonism, the treatment can include dopaminergic drugs (these are commonly recommended for those who have been diagnosed with Parkinson’s disease). One of the most recommended dopaminergic drugs is levodopa, providing successful results in patients who are suffering from tremors, associated with speech and swallowing difficulties.
Prognosis
In general, the prognosis of this condition is negative. There are patients who will not survive the changes brought on by this condition. Others can recover completely from the condition, while some will become disabled. Severe disability is a serious possibility – however, the disabilities can cover a wide range, starting with minor tremors or ataxia and going as far as spastic paralysis affecting all the limbs or even the locked-in syndrome. In general, the recovery process is influenced by how extensive the damage was at the level of the brainstem (how many axons have suffered from demyelination).
It is believed that the prognosis for this condition was improved due to the advancements of the imagining techniques and also due to the early diagnosis. The biggest challenges that come during the recovery period are related to a person’s degree of independence, as well as to the motor skills and speech. Often times, the recovery is prolonged, due to the patient suffering from emotional instability and also from forgetfulness.
Patients need to understand that the recovery from the central pontine myelinolysis is a long and difficult process. The changes that occur might be permanent, leading to chronic disabilities or they may take a very long time to subside. During this period, psychological counseling is highly important – it can help the patient maintain an optimist focus and fight to get better. Depending on the extent of the damage, some patients might require specialized assistance. Often times, the personal assistant will provide the necessary assistance with daily tasks, such as the ones related to personal hygiene, dressing and feeding.
Pictures